Vision
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for more than 4.9 million confirmed cases and 328,000 deaths worldwide, and over a period of a few months. The numbers continue to rise. The US has reported more coronavirus deaths than any other country. The novel coronavirus has devastated our society and our economy.
As biomedical scientists, our skills have perhaps never been more acutely relevant than at this time. At Weill Cornell, we have some of the most prominent international experts in immunology and infectious disease. Given the urgent need to contribute to the finding of a solution in this crisis, we have established a task force that will allow us to join forces.
We know little about this disease. Our goal is to understand how the immune system responds to SARS-CoV-2. Our collective efforts to address this pandemic will strengthen existing connections within the Weill Cornell Immunology community, streamline our investigations, and build new endeavors as we all work to end this public health crisis. By concentrating our strengths, creativity and expertise, we can forge a path forward towards urgently needed treatments and vaccines.
Important questions about the immune response to COVID-19
1) What are the immune correlates of severe disease versus resolution of COVID-19?
2) What is the basis for the increased susceptibility of the older population to COVID-19? Is it the underlying medical conditions or is it a function of age itself?
3) Why are children at a lower risk for COVID-19 than adults? What role do children play in the spread of COVID-19?
4) How do racial and socio-economic backgrounds impact disease severity and underlying immunologic features?
5) How do underlying medical conditions increase the risk for serious illness with COVID- 19? This includes obesity, autoimmune disease, IBD and cancer.
6) How does the immune system allow an asymptomatic carrier/spreader state? What are the immune parameters that establish the state of “super-spreader”?
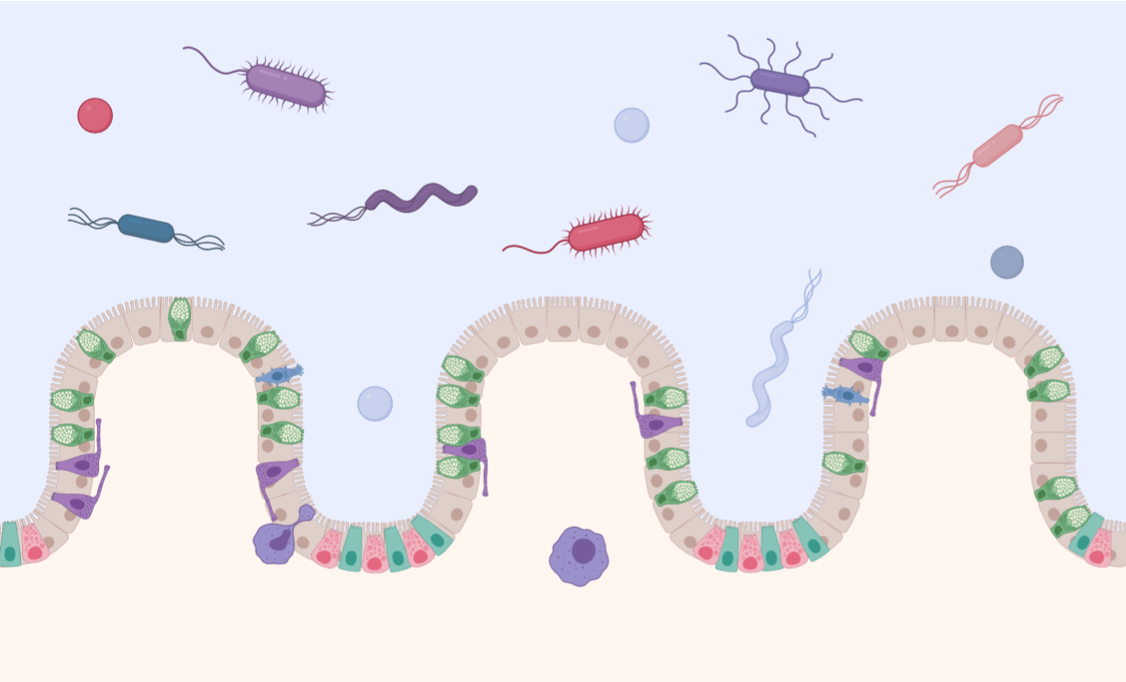
7) What is the contribution of barrier tissue versus systemic immunity to SARS-CoV-2?
8) Are there genetic factors that predispose or protect against infection and/or severe disease progression?
9) What is the basis of immunity to COVID-19 in the short-term versus the long term?
10) How does the florid inflammation (cytokine storm) seen in some patients correlate with anti-COVID-19 immunity and/or affect the development of anti-COVID-19 immunity?
11) What role does the immune system play in fatigue and frailty in patients with moderate and severe COVID-19?
12) Do signals derived from the microbiota influence anti-COVID-19 immune responses and/or susceptibility to infection and severe disease?
Bench to Clinic - What are we going to do against COVID-19?
Development of new anti-virals
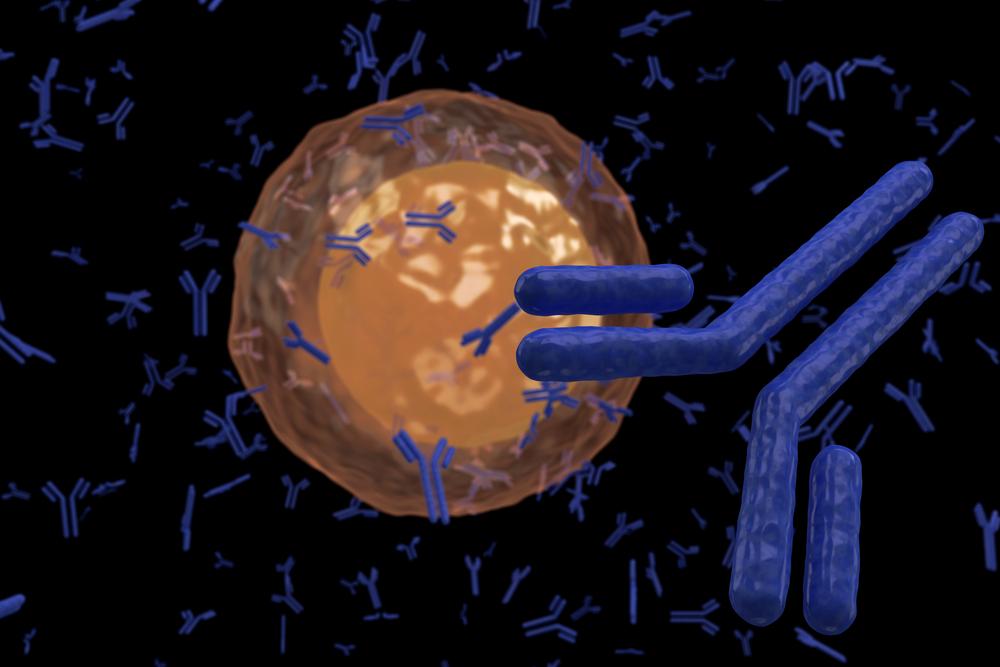
Development of SARS-CoV-2-specific antibody therapies
Development of cell-based therapies
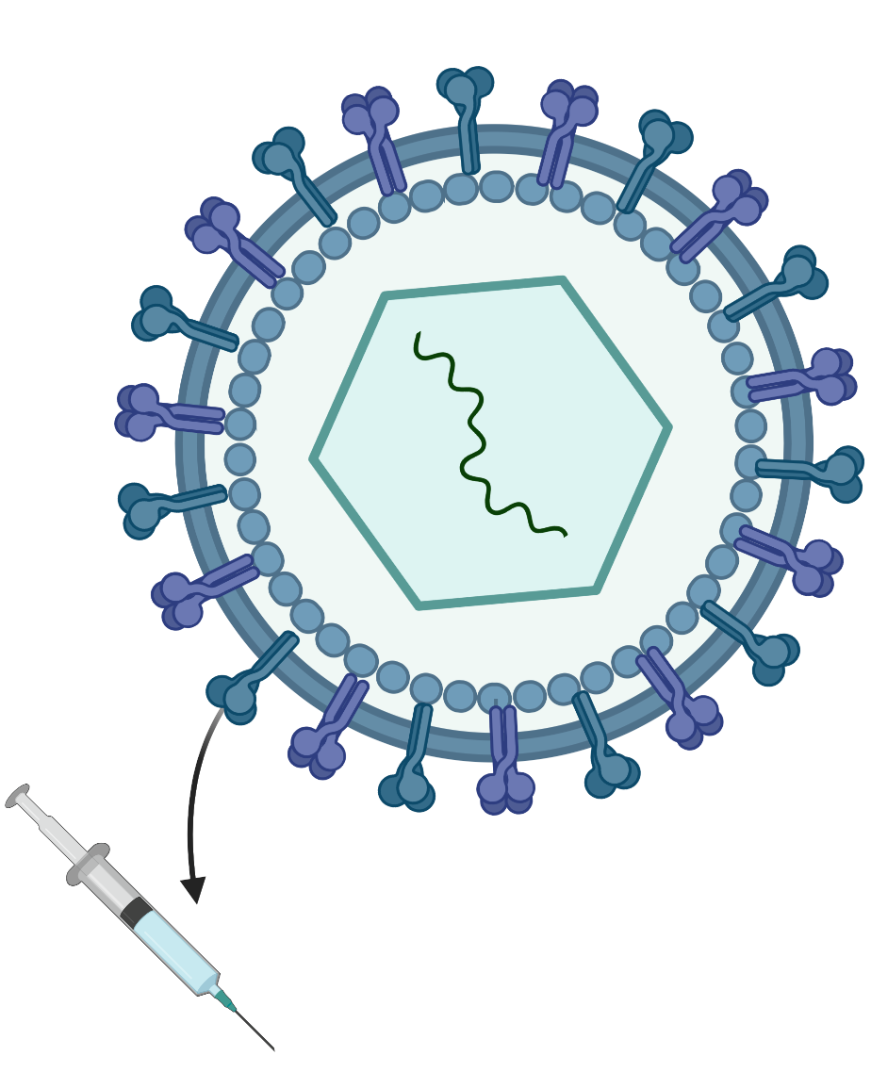
Development of new vaccines
Development of tailored therapies specific to each underlying comorbidity
Development of microbiome-based therapies
Biomarker Discovery
Faculty Research Interests
Vaccine Development
Anandasabapathy Laboratory
We study adaptive immunity (memory formation/persistence), and barrier defense to cancer and infection. We translate these findings to expand vaccines and cancer surveillance (skin and lung). As part of these efforts we have studied the smallpox vaccine, and Dendritic Cell-targeted viral and cancer vaccines and adjuvants for over a decade. We are interested in how SARS-CoV-2 impacts Dendritic Cell function/antigen presentation, Type I and Type II IFN pathways, and to define correlates of protective immunity. We would like to contribute to studying the human immune response (and variance), using human immune monitoring and functional genomics approaches to better define the pathophysiology of SARS-CoV-2 directly ex vivo. Ideally, we would work closely with clinical collaborators on the front line.
Blander Laboratory
Our COVID-19 research is centered on testing a novel vaccine candidate, identifying CD8 T cell biomarkers of immune protection, and defining mechanisms of immune evasion and cell death by SARS-CoV-2. We are conducting this work with Weill Cornell Medicine labs of Brad Jones, Laura Santambrogio, Douglas Nixon and Robert Schwartz, Bettina Wagner at Cornell University, and the NYP-WELCOME COVID-19 study by Silvia Formenti, Virginia Pascual and Elizabeth Ross. Our unique contribution to science is discovering the innate immune system can sense microbial viability. We shifted focus in the field from a purely ‘what molecules are there’ to a ‘what is the threat level’ risk assessment of infection. Pathogen-associated molecular patterns (PAMPs) alert the immune system of an infection, but detection of vita-PAMPs signifies a live pathogen and heightens the threat level the immune system is faced with. Bacterial messenger RNA and cyclic dinucleotides are vita-PAMPs that we showed elicit particularly high levels of inflammation and immune protection. We also found that a strategy to block antigen presentation by clinically important viruses, as a means of evading killer CD8 T cells, serves as a proxy of viral viability. It triggers a danger signal in cells to mobilize unconventional traffic of antigen-presenting MHC class I molecules, and activates unique CD8 T cells that protect against the virus. We are positioned to make important discoveries at the leading edge of this frontier in immunology. We are working to incorporate vita-PAMPs and novel adjuvants in vaccines for superior protection against infectious diseases and cancer.
Cantley Laboratory
In collaboration with Blenis, Elemento, Schwartz, Chen Laboratories and with the following laboratories outside of WCM:TenOever (MSSM), Diamond (Washington U), Matthews(Bristol University, UK). Targeting cellular kinases as treatment for COVID-19. Most cellular processes in human tissues are regulated by Serine/Threonine or Tyrosine protein kinases. In our project, we will test the efficacy of a set of FDA-approved kinase inhibitors on SARS-CoV-2 infection, as well as on the immune response of the host. The set of inhibitors are being chosen based on a new system developed in the Cantley Laboratory for predicting upstream protein kinases for phosphorylation sites. The drugs that block SARS-CoV-2 infectivity as well as modulate the host’s immune response at therapeutically relevant doses will be advanced to clinical trials. In collaboration with Sheinberg Laboratory (MSKCC), the Cantley lab is examiningSARS-CoV-2-derived phosphorylated antigen presentation on MHC-I as a vaccine for COVID-19.
Cubillos-Ruiz, Ehrt, Schnappinger and Nathan Laboratories
Our team seeks to develop a new vaccine candidate for SARS-CoV-2 capable of inducing durable protection against this virus. Our scientific approach is based on one of the safest and most commonly administered vaccines worldwide: the Bacillus Calmette-Guerin (BCG), which is the current vaccine for tuberculosis. Immunization with BCG has been shown to provide cross-protection against other respiratory infections, and it is currently associated with decreased incidence and severity of COVID-19 disease globally. Therefore, our team is exploiting these crucial features to create and test a series of genetically engineered BCG versions that stably express SARS-CoV-2 antigens. We envision that immunization using this unique approach will induce specific, potent and long-lasting protection against SARS-CoV-2, hence preventing future COVID-19 outbreaks and potential pandemic waves. Importantly, these modified BCG strains can be manufactured and scaled up for global vaccination purposes in a short timeframe and at low cost. Our immediate goal is to use various in vitro and in vivo model systems to evaluate if our vaccine prototypes can stimulate the production of protective antibodies that block infection of host cells by SARS-CoV-2.
Drug Discovery
Cantley Laboratory
In collaboration with Blenis, Elemento, Schwartz, Chen Laboratories and with the following laboratories outside of WCM:TenOever (MSSM), Diamond (Washington U), Matthews(Bristol University, UK). Targeting cellular kinases as treatment for COVID-19. Most cellular processes in human tissues are regulated by Serine/Threonine or Tyrosine protein kinases. In our project, we will test the efficacy of a set of FDA-approved kinase inhibitors on SARS-CoV-2 infection, as well as on the immune response of the host. The set of inhibitors are being chosen based on a new system developed in the Cantley Laboratory for predicting upstream protein kinases for phosphorylation sites. The drugs that block SARS-CoV-2 infectivity as well as modulate the host’s immune response at therapeutically relevant doses will be advanced to clinical trials. In collaboration with Sheinberg Laboratory (MSKCC), the Cantley lab is examiningSARS-CoV-2-derived phosphorylated antigen presentation on MHC-I as a vaccine for COVID-19.
Ma Laboratory
We study host-pathogen (influenza virus and parasites) and host-tumor interactions and the immune responses that ensue, as well as ways to modulate the immune responses to eliminate the infectious agent and repair infection-induced tissue damage. In particular, we study progranulin, a cytokine that has anti-inflammatory properties against infection induced cytokines and chemokines in the lungs. We also study a proprietary, highly selective and reversible small molecule inhibitor of the immunoproteasome in animal models of inflammatory diseases such as colitis. Progranulin and the unique immunoproteasome inhibitor could potentially be used in therapy to lessen SARS-CoV-2-induced immunopathology and death of patients.
Melnick Laboratory
The success of vaccines, and effective protection against recurrent infections in general, is dependent on the generation and maintenance of immunological memory, in the form of long-lived plasma cells and Memory B (MB)-cells. MB cells constitute a heterogeneous and quiescent population, poised to quickly respond to antigen upon recall, to provide elevated titers of further specified antibodies. We have defined mechanisms through which somatic mutations in epigenetic regulatory proteins induce lymphomagenesis. Our results show that modulating the primary immune responses through these epigenetic and transcriptional mechanisms in animals results in markedly higher immunoglobulin gene diversity, which could potentially lead to more effective formation of neutralizing antibodies able to clear infections and prevent future re-infections. We have defined specific druggable targets on the regulatory proteins that control this immunoglobulin diversification process. We predict that it will be similarly possible to generate small molecules against these protein domains. We postulate that transient inhibition of these targets can dramatically enhance the humoral immune response to Coronavirus, in the context of primary infections or vaccinations, to favor the development of long-lived MB cells with an extended immunoglobulin gene repertoire. We predict such MB populations would boost the response to ensuing infections with the same or even closely-related virus strains. This approach could enable even cancer patients with impaired humoral immune systems to develop natural immunity to these or other related pathogens.
Mendias Laboratory
We are a translational lab, studying basic biological mechanisms of skeletal muscle and connective tissue growth and remodeling, and applying these to observational studies and clinical trials in patients. A particular focus of our lab is the prevention of skeletal muscle atrophy following injury and disease. Many patients with moderate and severe COVID-19 develop prolong weakness and frailty. The immune system appears to trigger proteolysis in skeletal muscle to mobilize amino acids and energy stores to fuel expansion of immune cell populations and combat acute infection. In patients who experience the most severe frailty and atrophy, immune-mediated muscle proteolysis seems to continue long after the infection has cleared. Previous studies have identified a correlative role of the immune system in inducing muscle atrophy in SARS and MERS patients, although this is unknown in COVID-19 patients. In collaboration with WCM Pathology, we are studying muscle biopsies of COVID-19 patients to identify the nature of weakness and frailty in this disease. We hope these studies will help inform the acute rehabilitation of patients recovering from COVID-19, and identify biological targets for potential interventional trials to restore strength and function.
Rogatsky Lab
The focus of the Rogatsky laboratory is on the transcriptional and epigenetic control of inflammation, particularly on the mechanisms that regulate inflammatory gene expression programs in macrophages. We have been successful at using genetic, genomic and pharmacological means to manipulate RNA polymerase (Pol) II transcription complexes to achieve specific changes in gene expression, which in vivo resulted in dramatic improvements in several mouse models of autoinflammatory diseases. We are interested in dissecting the role of macrophages in SARS-CoV-2-induced acute respiratory distress syndrome (ARDS), the main driver of COVID19-associated mortality. We are testing small-molecule inhibitors of Pol II transcription complexes for their ability to modulate type I interferon and inflammatory pathways in monocytes/macrophages. We are also interested in establishing mouse models of SARS-CoV-2-induced ARDS to test these compounds in preclinical and ultimately translational studies.
Schwartz/Chen Laboratory
Innate Immunity
Barrat Laboratory
Role of plasmacytoid dendritic cells (pDCs) in the pathogenesis of the COVID-19 disease
It has been reported that in patients in critical condition, SARS-CoV-2 can trigger a robust inflammatory response in the lungs that is often referred as a “cytokine storm”. Although some of the pro-inflammatory mediators have been identified (IL-6, TNF, IL-1s etc…), it is unclear why some patients develop such an inflammatory response to the virus and what is the mechanism of activation of the cells, likely macrophages, producing these mediators. Interestingly, similar acute lung injury has been described in SARS and MERS patients. Plasmacytoid dendritic cells (pDCs) have been shown to produce large amount of type I interferon (IFN-I) in response to these viruses and using preclinical models of SARS, it was shown that depleting pDCs or blocking IFN-1 could prevent disease suggesting that pDCs could have a detrimental role in promoting the inflammatory response in response to the virus. Furthermore, ACE2 is a protein that is important to allow the entry SARS-CoV-2 in the cells and reports indicate that ACE2 can be upregulated by IFN-I. Our lab is investigating whether pDCs can be directly activated by SARS-CoV-2, the mechanism by which pDCs can sense the virus and whether the IFN-I produced by these cells can contribute to the recruitment and activation of inflammatory macrophages in the lung of patients. Understanding how pDCs respond to SARS-CoV-2 and whether these cells promote the cytokine storm could open news way to intervene for the benefit of patients.
Blander Laboratory
We study the fundamental principles of innate and adaptive immunity to design new therapies and vaccines. We would like to test vaccine candidates for COVID-19, study CD8 T cell responses in COVID-19, and define potential mechanisms of innate immune evasion and cell death by SARS-CoV-2. We are interested in understanding how the immune system allows an asymptomatic carrier/spreader state, the contribution of barrier tissue versus systemic immunity to SARS-CoV-2, and development of protective vaccines. Access to COVID-19 tissues and development of mouse models will be invaluable for our efforts. We welcome collaborations and are so far working with several Weill Cornell Faculty including Formenti, Demaria, Santambrogio, Loda, Inghirami, Nixon and Schwartz.
Demaria Laboratory
It is expected that many cancer patients will become infected by SARS-CoV-2 and it is essential to understand the interplay of the virus, the immune system and the tumor. A high neutrophil to lymphocyte ratio (NLR) is relatively frequent in patients with some advanced solid malignancies, and is associated with worse outcome. Lymphopenia in cancer patients is also common, often as a result of treatment, and when persistent is usually a negative prognostic indicator. Lymphopenia and high NLR have also been reported in SARS-CoV-2 infected patients. The degree of lymphopenia is associated with disease severity. The exuberant inflammation and immune exhaustion have been hypothesized as causes of the lymphopenia, but the cell subsets most affected and the pathogenesis of lymphopenia remain poorly understood. These observations raise concerns about the risk of severe COVID19 disease in cancer patients, and the modulation of this risk by cancer treatment, including radiotherapy and immunotherapy. Thus, it is critical to better understand the pathogenesis of SARS-CoV-2-driven lymphopenia, and to study whether the immune dysregulation pre-existing in cancer patients alters the development of the immunological changes caused by the infection. As a first step, we plan to investigate possible mechanisms contributing to SARS-CoV-2-driven lymphopenia using in vitro models as well as patients blood and tissue. This hypothesis-generating work will provide the rationale for testing experimentally candidate molecular mechanisms. In parallel, we are interested in understanding whether SARS-CoV-2 infects ACE2-positive cancer cells and can alter the tumor immune contexture.
Formenti Laboratory
Formenti and Marciscano in the Division of Experimental Radiotherapy of the Department of Radiation Oncology are studying the potential to use very low-dose radiation therapy (VLD-RT) as an anti-inflammatory treatment to minimize inflammation and lung injury caused by the SARS-CoV-2 (COVID-19) coronavirus. It has become increasingly clear that the body’s immune response to the virus can become dysregulated leading to life-threatening lung inflammation known as acute respiratory distress syndrome (ARDS). Treatments designed to limit excessive inflammation may help improve outcomes for patients during the COVID-19 pandemic. Historically, VLD-RT was administered to the lungs of patients with severe viral pneumonia that did not respond to standard therapies. Following treatment with VLD-RT, a significant proportion of patients experience rapid improvement in their symptoms. There is now considerable interest in ‘repurposing’ VLD-RT to treat patients with severe pneumonia due to SARS-CoV-2 to prevent the development of ARDS. Human lung cell lines, organoids and in vivo models of severe viral pneumonia/ARDS will help us understand the immunological processes responsible for the immune-suppressive effects of VLD-RT.
We propose to focus on the study of alveolar macrophages (AMs), a potent immune cell population that resides in the respiratory units (alveoli) of the lungs. AMs are a major culprit in ARDS – whether VLD-RT can reprogram AMs towards an anti-inflammatory phenotype that results in less lung injury will be of interest. Furthermore, we will investigate whether VLD-RT modifies expression of ACE2, the receptor that SARS-CoV-2 uses to enter and infect human lung cells (type II pneumocytes).
Ivashkiv Laboratory
Our laboratory studies how molecules called interferons and cytokines activate the immune system and cause inflammation and tissue damage. We are particularly interested in an immune cell type called a macrophage and how it is activated to produce large amounts of cytokines such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor (TNF). The lab has primarily worked on macrophages and cytokines in autoimmune diseases such as rheumatoid arthritis and lupus. COVID-19 patients who deteriorate and require hospitalization and mechanical ventilation exhibit a hyperinflammatory state with activation of macrophages and high levels of IL-1, IL-6, TNF and other cytokines that drive inflammation and severe lung damage. In some patients very high cytokine levels, known as ‘cytokine storm’ contribute to mortality. Our research interests related to COVID-19 center around understanding how infection with SARS-CoV-2 activates macrophages and causes inflammatory cytokine production and cytokine storm. This work includes immune and inflammatory profiling of COVID-19 patients to identify risk factors for disease progression and identify new therapeutic targets. We are also collaborating on clinical trials of COVID-19 patients to identify mechanisms of action of novel therapeutics, and biomarkers for patient stratification and precision medicine approaches to therapy. In addition, in basic science projects we are investigating mechanisms by which SARS-CoV-2 activates macrophages to produce inflammatory cytokines. The goals of these studies are to identify strategies for preventing cytokine storm while preserving the ability of the immune response to combat and eliminate SARS-CoV-2.
Josefowicz Laboratory
Epigenetic Priming of Inflammatory Genes in COVID-19: Insights into Pathogenesis, Prognosis, and Consequences. A major priority is to understand the inflammatory pathology of COVID-19. The urgent applications of that knowledge would include identification of novel therapeutic targets, risk stratification especially among those that are otherwise young and healthy, and guiding of existing experimental therapies such as cytokine blockade. Our approach is to profile epigenetic priming of inflammatory genes in immune cells using low cell number epigenomics, with the hypothesis that epigenetic “poising” at inflammatory genes contributes to COVID-19 course. We have already established this workflow in studies of inflammatory arthritis (collaboration with Virginia Pascual) to study the relationship between inflammatory gene poising and disease states and responsiveness to immune therapies, and also to understand the range of epigenetic poising of inflammation among healthy donors and across age and sex. These studies focus on underlying mechanisms of inflammatory pathology and their long-term sequelae with relevance extending beyond COVID-19 to a broad array of disease states, including other respiratory infections, ARDS, and inflammatory disease, and what we learn could have long-term benefit across a range of conditions.
Monticelli Laboratory
Using an integrative approach that bridges innate immunity and cellular metabolism, our lab is focused on examining how tissue-specific signals from innate immune system can be harnessed to limit pathologic inflammation and promote beneficial tissue repair in the lung. For example, we previously identified a pathway of lung epithelial repair orchestrated by a unique population of innate lymphoid cells during severe viral infection which may have relevance to SARS-CoV-2 infection. Using both patient samples and murine models, we are interested in 1) characterizing the pathologic immune cell infiltration in patients infected with SARS-CoV-2, 2) examining the relationship between this immune cell infiltration and the progression of lung epithelial damage during SARS-CoV-2 infection, 3) identifying the signals and key molecules produced by the innate lymphoid cells that can be used to promote restoration of lung tissue function, improve oxygenation, or limit cytokine storms.
Ndhlovu Laboratory
My research program uses single cell and immuno-epigenetic approaches to resolve molecular mechanisms regulating viral entry of SARS-CoV-2 infection across various tissues and cell types and seeks to identify therapeutic host targets that influence disease pathogenesis and reduce morbidity and mortality and relieve the burden of this infection.
Nixon Laboratory
My lab is interested in collaborating on basic host pathogen interactions in the context of SARS-CoV-2 and HIV co-infection, and on the genetics of COVID-19 susceptibility and disease progression. We also have used connectivity mapping for drug repurposing studies in COVID-19. We are also interested in how innate iNKT and MAIT immune cells might contribute to pathogenesis or protection.
Pascual Laboratory
Virginia Pascual’s group is working on an NIAID Supplement to 5 U01 AI1131386-03 (High Precision Systems Analysis of Infant Immune Responses; O. Ramilo P.I. Nationwide, Columbus, OH; V Pascual, Co-I): This supplement intends to recruit 200 pregnant mother-infant pairs in the US and Central America (Panama), where a network of pediatricians involved in maternal-fetal immune monitoring is already in place. The goal of this proposal is to comprehensively characterize the clinical, immunologic, viral variables and outcomes of COVID-19 infection in mother-infant pairs and to assess the development of the immune system during the 1st year of life. We are also working on a collaboration with Steve Josefowicz’s group to examine the role of “Trained Immunity” in predisposition to severe COVID-19 outcome. The proposal is based on preliminary data obtained as a collaboration between our labs addressing how epigenetic reprogramming of innate immune precursors might predispose children with autoinflammatory diseases to exaggerated responses to subsequent inflammatory triggers. The hypothesis is that COVID-19 patients suffering from “cytokine storms” are epigenetically predisposed to innate immunity-related morbidity. Finally, we are involved in the development phase of “WelCoME-C: Weil Cornell Medicine Employees Cohort”. This protocol, led by Silvia Formenti, intends to develop a longitudinal cohort to capture Weill-Cornell Medicine employees through SARS-CoV-2 exposure. The goals are to integrate clinical, laboratory, virus-related factors, demographics and comorbidities. Importantly, it will acquire and store samples for viral studies, genetic associations as well as immune monitoring to identify predictors of outcomes.
Santambrogio Laboratory
Several factors control the outcome of host–viral interactions with host factors being pivotal to both innate and adaptive immunity. Among the host factors that control the end-result of viral infection MHC alleles polymorphism play a fundamental role. The focus of our research will be the characterization of the MHC I and MHC II SARS-CoV-2 immunopeptidome across human ACE2 positive epithelial and endothelial cells as well as professional antigen presenting cells, such as Dendritic Cells which, phagocytose SARS-CoV-2 infected cells and cross-present the antigens to T cells. The ultimate goal would be to comparatively and quantitatively map the differential MHC-restricted immunopeptidome presented by infected cells across different human haplotypes. The top identified antigenic peptides will be tested for recognition by T cells to determine the nature of the T cell response to viral antigens, and to test the hypothesis that certain MHC haplotypes may be protective or conducive of COVID-19 clinical outcome. A well know mechanism of viral escape is the viral interference with the MHC I antigen processing and presentation machinery which generates viral peptides for adaptive immune responses. Indeed, MHC-I viral peptides can stimulate CD8+ cytotoxic T lymphocytes (CTLs), which play a critical role in the defense against viral infections. As part of this project we will also investigate the possibility that SARS-CoV-2 interferes with the proteasome/immunoproteasome or the MHC I assembly trafficking and presentation machinery. Overall, the proposed studies will provide critical information about potential mechanisms of immune escape of SARS-CoV-2.
Schwartz Laboratory
In collaboration with Shuibing Chen/Todd Evans Laboratories. We focus on human embryonic stem cell/induced pluripotent stem cell (hESC/iPSC)-based disease modeling and drug discovery. We have expertise in generating a variety of human cells and organoids and have developed a platform of cell and tissue derivatives from ten different organs including the pancreas, heart, liver, intestines, and lungs. Using our organoid platforms, our collective labs have now systematically probed which cell types are permissive to SARS-CoV-2 infection using a SARS-CoV-2 pseudoparticle, and in collaboration with Benjamin TenOever at Mount Sinai, the SARS-CoV-2 virus. We have completed transcriptomic analysis following SARS-CoV-2 infection of hPSC-derived cell types. We have performed a high throughput drug screen using hPSC-derived organoids and are validating this currently in cell-based and animal models. We plan to identify potent drugs that interact and/or alter host factors or directly target the virus itself to help mitigate disease. We are obtaining primary clinical tissue material (IRB approved) and awaiting patient clinical materials (IRB approved) to characterize early and late disease using a variety of tools to understand the acute (transcriptomic, proteomic, phosphoproteomic) and chronic changes (transcriptomic, ATAQ-seq) that occur in several tissues/cells as a consequence of SARS-CoV-2 infection. This collective work is in collaboration with several lab groups including Cantley/Nixon/Ndhlovu as well as other colleagues.
Human Immune Profiling
Anandasabapathy Laboratory
We study adaptive immunity (memory formation/persistence), and barrier defense to cancer and infection. We translate these findings to expand vaccines and cancer surveillance (skin and lung). As part of these efforts we have studied the smallpox vaccine, and Dendritic Cell-targeted viral and cancer vaccines and adjuvants for over a decade. We are interested in how SARS-CoV-2 impacts Dendritic Cell function/antigen presentation, Type I and Type II IFN pathways, and to define correlates of protective immunity. We would like to contribute to studying the human immune response (and variance), using human immune monitoring and functional genomics approaches to better define the pathophysiology of SARS-CoV-2 directly ex vivo. Ideally, we would work closely with clinical collaborators on the front line.
Artis Laboratory
We study the regulation of innate and adaptive immunity at the body’s barrier surfaces, including the airway and intestine, in the context of infection, inflammation and tissue repair. We also employ experimental techniques to examine how the microbiota that colonize these barrier surfaces influence immunity and inflammation. In the context of anti-viral immunity, we previously identified a critical role for signals derived from the microbiota in promoting innate and adaptive immunity to influenza, LCMV and norovirus. Given the high levels of SARS-CoV-2 in the human intestine along with expression of receptors for cell entry, we would propose to study associations between microbial diversity within the microbiota of patients and susceptibility to SARS-CoV-2 infection and disease severity. We also established the Roberts Institute Live Cell Bank that routinely collects clinical data, matched blood, intestinal biopsies and microbiota samples. This resource could be applied to multiple SARS- CoV-2 studies.
Blander Laboratory
We study the fundamental principles of innate and adaptive immunity to design new therapies and vaccines. We would like to test vaccine candidates for COVID-19, study CD8 T cell responses in COVID-19, and define potential mechanisms of innate immune evasion and cell death by SARS-CoV-2. We are interested in understanding how the immune system allows an asymptomatic carrier/spreader state, the contribution of barrier tissue versus systemic immunity to SARS-CoV-2, and development of protective vaccines. Access to COVID-19 tissues and development of mouse models will be invaluable for our efforts. We welcome collaborations and are so far working with several Weill Cornell Faculty including Formenti, Demaria, Santambrogio, Loda, Inghirami, Nixon and Schwartz.
Chen-Kiang Laboratory
Chen-Kiang Laboratory in collaboration with Elemento and Inghirami Labs Our translational research is focused on uncovering the clonal heterogeneity and evolution in lymphoma cells, changes in the immune landscape and tumor-immune interaction in the context of clinical responses to several clinical trials targeting CDK4/6 in lymphoma. We characterize serial specimens from individual patients unbiasedly by longitudinal integrated functional genomics at the single cell resolution, including single cell (sc)RNA-sequencing and multiplex analysis with immunohistochemistry and with CyTOF. Our ultimate goal is to identify genomic drivers that discriminate sensitivity from resistance to our hypothesis-driven therapies in lymphoma and develop cost-effective assays for biomarkers that are applicable in pathology labs. We hope to make a meaningful contribution to collaborative COVID-19 research, leveraging our substantial cumulative scRNA-sequencing data on the immune landscape in humans, and our experience in coupling genomic data with annotated clinical data. Our particular interests relate to “What are the immune correlates of severe disease versus resolution of COVID-19?” and how impairment in the immune system by cancer exacerbates disease severity in COVID-19.
Demaria Laboratory
It is expected that many cancer patients will become infected by SARS-CoV-2 and it is essential to understand the interplay of the virus, the immune system and the tumor. A high neutrophil to lymphocyte ratio (NLR) is relatively frequent in patients with some advanced solid malignancies, and is associated with worse outcome. Lymphopenia in cancer patients is also common, often as a result of treatment, and when persistent is usually a negative prognostic indicator. Lymphopenia and high NLR have also been reported in SARS-CoV-2 infected patients. The degree of lymphopenia is associated with disease severity. The exuberant inflammation and immune exhaustion have been hypothesized as causes of the lymphopenia, but the cell subsets most affected and the pathogenesis of lymphopenia remain poorly understood. These observations raise concerns about the risk of severe COVID19 disease in cancer patients, and the modulation of this risk by cancer treatment, including radiotherapy and immunotherapy. Thus, it is critical to better understand the pathogenesis of SARS-CoV-2-driven lymphopenia, and to study whether the immune dysregulation pre-existing in cancer patients alters the development of the immunological changes caused by the infection. As a first step, we plan to investigate possible mechanisms contributing to SARS-CoV-2-driven lymphopenia using in vitro models as well as patients blood and tissue. This hypothesis-generating work will provide the rationale for testing experimentally candidate molecular mechanisms. In parallel, we are interested in understanding whether SARS-CoV-2 infects ACE2-positive cancer cells and can alter the tumor immune contexture.
Formenti Laboratory
Formenti and Marciscano in the Division of Experimental Radiotherapy of the Department of Radiation Oncology are studying the potential to use very low-dose radiation therapy (VLD-RT) as an anti-inflammatory treatment to minimize inflammation and lung injury caused by the SARS-CoV-2 (COVID-19) coronavirus. It has become increasingly clear that the body’s immune response to the virus can become dysregulated leading to life-threatening lung inflammation known as acute respiratory distress syndrome (ARDS). Treatments designed to limit excessive inflammation may help improve outcomes for patients during the COVID-19 pandemic. Historically, VLD-RT was administered to the lungs of patients with severe viral pneumonia that did not respond to standard therapies. Following treatment with VLD-RT, a significant proportion of patients experience rapid improvement in their symptoms. There is now considerable interest in ‘repurposing’ VLD-RT to treat patients with severe pneumonia due to SARS-CoV-2 to prevent the development of ARDS. Human lung cell lines, organoids and in vivo models of severe viral pneumonia/ARDS will help us understand the immunological processes responsible for the immune-suppressive effects of VLD-RT.
We propose to focus on the study of alveolar macrophages (AMs), a potent immune cell population that resides in the respiratory units (alveoli) of the lungs. AMs are a major culprit in ARDS – whether VLD-RT can reprogram AMs towards an anti-inflammatory phenotype that results in less lung injury will be of interest. Furthermore, we will investigate whether VLD-RT modifies expression of ACE2, the receptor that SARS-CoV-2 uses to enter and infect human lung cells (type II pneumocytes).
Lipkin, Hassane and Elemento Laboratories
The presence of clonal hematopoiesis (CH) supports a hyperinflammatory state with elevated cytokines, including IL-1 and IL-6. Preliminary analysis of macrophages in the lungs of COVID-19 patients with severe disease revealed the presence of more inflammatory macrophages. We hypothesize that CH may underlie the higher incidence of hyperinflammation in susceptible individuals and lead to adverse outcome in COVID-19 patients. We will work to delineate the risk associated with different CH genotypes for COVID-19 related immune-inflammation and elucidate worse clinical outcomes with CH mutations and COVID-19, accounting for lung disease and other predisposing co-morbidities. Finally, to more directly assess the impact on immune-inflammation, we will correlate CH status with plasma cytokine levels (e.g. IL-6).
Inghirami Laboratory
Our laboratory focuses on dissecting the molecular mechanisms of lymphoid transformation and on identifying the contribution of the host-elements in lymphoid maturation, expansion and viral-tumor immune control. Our research is focused on two directions:
a) Profile serial immune responses using peripheral blood mononuclear cells (PBMC) obtained from SARS-CoV-2-positive individuals (no comorbidities and with cancer) using multicolor flow cytometry, functional and genomic testing (NSG IgH and TCRa/b sequencing). We will take advantage of our existing algorithms to define clonal evolution, and assess the SARS-CoV-2 peptide binding of B- and T-cells. Further studies will determine the binding profile of SARS-CoV2 IgG against a library of recombinant proteins, corresponding to all coding regions of the SARS-CoV2. Predicted anti-SARS-CoV-2 TCR will be cloned and functionally characterized.
b) Generate of an “agnostic” library of human antibodies recognizing multiple SARS-CoV-2 protein epitopes on the viral surface capsid. SARS-CoV-2 specific IgG+ B-cells from convalescent patients (leukapheresis) will be fused to a non-secreting murine myeloma partner to generate human B-cell hybridomas. SARS-CoV-2-specific antibodies will be tested to assess for their binding to Coronovirus proteins (recombinant proteins of 229E, NL63, OC43, HKU1, MERS-CoV, SARS-CoV and SARS-CoV2) and their efficacy in blocking the viral attachment and entry of pseudotyping and natural SARS-CoV-2 to lung epithelial Calu-3 cells.
Ivashkiv Laboratory
Our laboratory studies how molecules called interferons and cytokines activate the immune system and cause inflammation and tissue damage. We are particularly interested in an immune cell type called a macrophage and how it is activated to produce large amounts of cytokines such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor (TNF). The lab has primarily worked on macrophages and cytokines in autoimmune diseases such as rheumatoid arthritis and lupus. COVID-19 patients who deteriorate and require hospitalization and mechanical ventilation exhibit a hyperinflammatory state with activation of macrophages and high levels of IL-1, IL-6, TNF and other cytokines that drive inflammation and severe lung damage. In some patients very high cytokine levels, known as ‘cytokine storm’ contribute to mortality. Our research interests related to COVID-19 center around understanding how infection with SARS-CoV-2 activates macrophages and causes inflammatory cytokine production and cytokine storm. This work includes immune and inflammatory profiling of COVID-19 patients to identify risk factors for disease progression and identify new therapeutic targets. We are also collaborating on clinical trials of COVID-19 patients to identify mechanisms of action of novel therapeutics, and biomarkers for patient stratification and precision medicine approaches to therapy. In addition, in basic science projects we are investigating mechanisms by which SARS-CoV-2 activates macrophages to produce inflammatory cytokines. The goals of these studies are to identify strategies for preventing cytokine storm while preserving the ability of the immune response to combat and eliminate SARS-CoV-2.
Jones Laboratory
We are a viral immunology lab primarily focused on studying the T cell response to HIV infection, and mechanisms of viral persistence on antiretroviral therapy. We interested in studying how the magnitudes, functionalities, and immunodominance patterns of CD4+ and CD8+ T cell responses to SARS-CoV-2 relate to disease severity and outcome. We are also interested in characterizing the viral dynamics of early SARS-CoV-2 infection in tandem with the cellular immune response. Our lab is also active in performing mouse studies involving replication competent HIV.
Josefowicz Laboratory
Epigenetic Priming of Inflammatory Genes in COVID-19: Insights into Pathogenesis, Prognosis, and Consequences. A major priority is to understand the inflammatory pathology of COVID-19. The urgent applications of that knowledge would include identification of novel therapeutic targets, risk stratification especially among those that are otherwise young and healthy, and guiding of existing experimental therapies such as cytokine blockade. Our approach is to profile epigenetic priming of inflammatory genes in immune cells using low cell number epigenomics, with the hypothesis that epigenetic “poising” at inflammatory genes contributes to COVID-19 course. We have already established this workflow in studies of inflammatory arthritis (collaboration with Virginia Pascual) to study the relationship between inflammatory gene poising and disease states and responsiveness to immune therapies, and also to understand the range of epigenetic poising of inflammation among healthy donors and across age and sex. These studies focus on underlying mechanisms of inflammatory pathology and their long-term sequelae with relevance extending beyond COVID-19 to a broad array of disease states, including other respiratory infections, ARDS, and inflammatory disease, and what we learn could have long-term benefit across a range of conditions.
Longman laboratory
Our laboratory has experience in immunophenotyping and microbiome analysis of patients with inflammatory bowel disease (IBD). Diarrhea and GI symptoms are common presenting symptoms of COVID-19, but the impact on intestinal homeostasis, the effect on underlying IBD, and the interaction with immunosuppressive medications is not known. We have developed longitudinal clinic-based treatment cohorts that can be used to examine these questions in patients with IBD.
Lu Laboratory
Our lab studies how immune cells modulate and are modulated by tissue-resident cells, with a focus on understanding rheumatic diseases such as lupus, where patients develop skin lesions in the sun and this can trigger an increase in their autoimmune responses. We are interested in how inflammation in the skin and other tissues can modulate immune responses that begin in lymphoid organs such as lymph nodes and tonsils. We are interested in how inflammation in COVID-19 infections impacts immune responses initiated in lymphoid organs and how understanding COVID-19 can inform and be informed by understanding of rheumatic diseases.
Monticelli Laboratory
Using an integrative approach that bridges innate immunity and cellular metabolism, our lab is focused on examining how tissue-specific signals from innate immune system can be harnessed to limit pathologic inflammation and promote beneficial tissue repair in the lung. For example, we previously identified a pathway of lung epithelial repair orchestrated by a unique population of innate lymphoid cells during severe viral infection which may have relevance to SARS-CoV-2 infection. Using both patient samples and murine models, we are interested in 1) characterizing the pathologic immune cell infiltration in patients infected with SARS-CoV-2, 2) examining the relationship between this immune cell infiltration and the progression of lung epithelial damage during SARS-CoV-2 infection, 3) identifying the signals and key molecules produced by the innate lymphoid cells that can be used to promote restoration of lung tissue function, improve oxygenation, or limit cytokine storms.
Nixon Laboratory
My lab is interested in collaborating on basic host pathogen interactions in the context of SARS-CoV-2 and HIV co-infection, and on the genetics of COVID-19 susceptibility and disease progression. We also have used connectivity mapping for drug repurposing studies in COVID-19. We are also interested in how innate iNKT and MAIT immune cells might contribute to pathogenesis or protection.
Pascual Laboratory
Virginia Pascual’s group is working on an NIAID Supplement to 5 U01 AI1131386-03 (High Precision Systems Analysis of Infant Immune Responses; O. Ramilo P.I. Nationwide, Columbus, OH; V Pascual, Co-I): This supplement intends to recruit 200 pregnant mother-infant pairs in the US and Central America (Panama), where a network of pediatricians involved in maternal-fetal immune monitoring is already in place. The goal of this proposal is to comprehensively characterize the clinical, immunologic, viral variables and outcomes of COVID-19 infection in mother-infant pairs and to assess the development of the immune system during the 1st year of life.
We are also working on a collaboration with Steve Josefowicz’s group to examine the role of “Trained Immunity” in predisposition to severe COVID-19 outcome. The proposal is based on preliminary data obtained as a collaboration between our labs addressing how epigenetic reprogramming of innate immune precursors might predispose children with autoinflammatory diseases to exaggerated responses to subsequent inflammatory triggers. The hypothesis is that COVID-19 patients suffering from “cytokine storms” are epigenetically predisposed to innate immunity-related morbidity. Finally, we are involved in the development phase of “WelCoME-C: Weil Cornell Medicine Employees Cohort”. This protocol, led by Silvia Formenti, intends to develop a longitudinal cohort to capture Weill-Cornell Medicine employees through SARS-CoV-2 exposure. The goals are to integrate clinical, laboratory, virus-related factors, demographics and comorbidities. Importantly, it will acquire and store samples for viral studies, genetic associations as well as immune monitoring to identify predictors of outcomes.
Salvatore Laboratory
The clinical spectrum of COVID-19 is heterogeneous and ranges from asymptomatic disease to severe pneumonia and death. COVID-19 patients often have lymphopenia, elevated neutrophils, and increased levels pro-inflammatory cytokines and chemokines. Although age and comorbidities such as diabetes, hypertension and obesity are associated with severe illness, little is known about the determinants of the diverse outcomes. Subjects with hematologic malignancies and/or bone marrow or solid organ transplant are potentially susceptible to severe COVID19, but little is known about the natural history of disease in these patients. To understand the relative contribution of viral evolution and host factors to disease outcome, we built a cohort of patients with varying degree of disease severity that also includes patients with hematologic malignancies and after transplant (in collaboration with H Sing, C Vorkras, JM Hsu, WCM) and we are longitudinally collecting specimens for the comprehensive characterization of viral, epidemiological and immunological drivers of clinical outcome. Our aims are:
1. Profile and characterize cellular and humoral immune responses to SARS-CoV-2, including impact of the virus on immune system (in collaboration with G Inghirami, WCM).
2. Identify the relationships between type of specific immune responses (neutralizing and non-neutralizing antibody, T cells) and subsequent clinical course.
3. Understand the role of deleterious immune responses such as cross-reacting autoantibodies and overly robust cytokines/inflammatory responses in pathogenesis (in collaboration with L Santambrogio WCM and L Ivashkiv, M Crow, HSS).
4. Determine viral dynamics and time of shedding, in different patient populations. (collaboration with E Ghedin, NIH, C Mason, WCM)
Santambrogio Laboratory
Several factors control the outcome of host–viral interactions with host factors being pivotal to both innate and adaptive immunity. Among the host factors that control the end-result of viral infection MHC alleles polymorphism play a fundamental role. The focus of our research will be the characterization of the MHC I and MHC II SARS-CoV-2 immunopeptidome across human ACE2 positive epithelial and endothelial cells as well as professional antigen presenting cells, such as Dendritic Cells which, phagocytose SARS-CoV-2 infected cells and cross-present the antigens to T cells. The ultimate goal would be to comparatively and quantitatively map the differential MHC-restricted immunopeptidome presented by infected cells across different human haplotypes. The top identified antigenic peptides will be tested for recognition by T cells to determine the nature of the T cell response to viral antigens, and to test the hypothesis that certain MHC haplotypes may be protective or conducive of COVID-19 clinical outcome. A well know mechanism of viral escape is the viral interference with the MHC I antigen processing and presentation machinery which generates viral peptides for adaptive immune responses. Indeed, MHC-I viral peptides can stimulate CD8+ cytotoxic T lymphocytes (CTLs), which play a critical role in the defense against viral infections. As part of this project we will also investigate the possibility that SARS-CoV-2 interferes with the proteasome/immunoproteasome or the MHC I assembly trafficking and presentation machinery. Overall, the proposed studies will provide critical information about potential mechanisms of immune escape of SARS-CoV-2.
Sonnenberg Laboratory
The Sonnenberg Laboratory has substantial expertise in defining the cellular and molecular mechanisms by which host-microbe interactions augment immunity, inflammation, tissue homeostasis and cancer within the mammalian gastrointestinal tract. Particularly, we focus on how the mammalian immune system interacts with trillions of normally beneficial microbes, termed the microbiota, to support intestinal health. The recent SARS-CoV-2 pandemic has demonstrated that this infection is commonly associated with multiple gastrointestinal symptoms, such as loss of appetite, nausea, vomiting and diarrhea. Furthermore, the virus is regularly detected in the feces of infected patients. Therefore, we are actively interrogating: (i) How SARS-CoV-2 infection causes gastrointestinal disorders; (ii) Whether there are long-term immunologic or microbiologic changes in the human intestine following SARS-CoV-2 infection; and (iii) Can we develop novel therapeutic approaches to protect the gastrointestinal tract in the context SARS-CoV-2 infection and enhance protective immunity. These research efforts are in close collaboration with multiple investigators at the Roberts Institute for Research in IBD, the Department of Medicine, and the Division of Gastroenterology.
Microbiome
Artis Laboratory
We study the regulation of innate and adaptive immunity at the body’s barrier surfaces, including the airway and intestine, in the context of infection, inflammation and tissue repair. We also employ experimental techniques to examine how the microbiota that colonize these barrier surfaces influence immunity and inflammation. In the context of anti-viral immunity, we previously identified a critical role for signals derived from the microbiota in promoting innate and adaptive immunity to influenza, LCMV and norovirus. Given the high levels of SARS-CoV-2 in the human intestine along with expression of receptors for cell entry, we would propose to study associations between microbial diversity within the microbiota of patients and susceptibility to SARS-CoV-2 infection and disease severity. We also established the Roberts Institute Live Cell Bank that routinely collects clinical data, matched blood, intestinal biopsies and microbiota samples. This resource could be applied to multiple SARS-CoV-2 studies.
Cohen Laboratory
faculty including T Krisko and H Nicholls Krisko, and The Metabolic Phenotyping Core Obesity and diabetes are emerging as risk factors for severe COVID-19 complications. This may be related to the influence of obesity on immune function. Our laboratory has extensive experience in animal models of obesity and characterization of associated metabolic abnormalities, including type 2 diabetes and fatty liver disease. We also have extensively characterized the influence of the microbiome on obesity and glucose metabolism. We run the Metabolic Phenotypic Core Facility at WCM, which offers extensive characterization of energy homeostasis, glucose metabolism and body composition. We are well- positioned to examine the influence of COVID-19 on metabolism, as well as the influence of obesity on the course of COVID-19 in suitable mouse models.
Guo Laboratory
About 20% of COVID-19 patients have diarrhea as the first symptom, suggesting a compositional and functional change of their gut microbiota. We are a gut microbiome lab that uses genetic approaches to modulate gut microbiota and investigate how their genes, pathways, and metabolites affect host biology. We are interested to know how the viral infection modifies the gut microbiota at the molecular level that leads to diarrhea, and we seek to engineer the human gut microbiota for better protection against Covid-19 or to ameliorate COVID-19 related diarrhea. My group is also open to other collaboration opportunities as long as our expertise can contribute.
Iliev Laboratory and Worgall Laboratory
We will investigate the role of the mycobiome/lung fungal co-infection in development and rapid exacerbation (or lack of such) of COVID-19 disease. Patient sputum, lung aspirates and fecal samples will be used to uncover fungal players, fungal immune signatures and lipid metabolites associated with disease outcome. The study will benefit from several advanced mycobiome and immuno-mycology pipelines in the Iliev laboratory, lipid metabolism expertise and tools available in the Worgall Laboratory. Mechanisms of disease severity will be further investigated in mouse models.
Longman Laboratory
Our laboratory has experience in immunophenotyping and microbiome analysis of patients with inflammatory bowel disease (IBD). Diarrhea and GI symptoms are common presenting symptoms of COVID-19, but the impact on intestinal homeostasis, the effect on underlying IBD, and the interaction with immunosuppressive medications is not known. We have developed longitudinal clinic-based treatment cohorts that can be used to examine these questions in patients with IBD.
Sonnenberg Laboratory
The Sonnenberg Laboratory has substantial expertise in defining the cellular and molecular mechanisms by which host-microbe interactions augment immunity, inflammation, tissue homeostasis and cancer within the mammalian gastrointestinal tract. Particularly, we focus on how the mammalian immune system interacts with trillions of normally beneficial microbes, termed the microbiota, to support intestinal health. The recent SARS-CoV-2 pandemic has demonstrated that this infection is commonly associated with multiple gastrointestinal symptoms, such as loss of appetite, nausea, vomiting and diarrhea. Furthermore, the virus is regularly detected in the feces of infected patients. Therefore, we are actively interrogating: (i) How SARS-CoV-2 infection causes gastrointestinal disorders; (ii) Whether there are long-term immunologic or microbiologic changes in the human intestine following SARS-CoV-2 infection; and (iii) Can we develop novel therapeutic approaches to protect the gastrointestinal tract in the context SARS-CoV-2 infection and enhance protective immunity. These research efforts are in close collaboration with multiple investigators at the Roberts Institute for Research in IBD, the Department of Medicine, and the Division of Gastroenterology.
Zeng Laboratory
We are a gut microbiome immunology lab with a focus on neonatal immunity against infections and the immune response at the maternal-fetal/neonatal interface. We also have ongoing studies of the neonatal gut microbiome in both humans and mice. Our interests center on defining whether there are immune or gut microbiome components that modulate vertical transmission of SARS-CoV-2 from the mother to the fetus or newborn. Utilizing novel COVID-19 mouse models with either neutrophil deficiency or IgG deficiency, we would like to define the contribution of neutrophils and the role of non-neutralizing IgG in the “cytokine storm”. In understanding why children have mild symptoms of SARS-CoV-2 infection, we plan on exploring potential unique gut microbiome-derived factors that confer protection in children. We are interested in the role of the gut microbiome in SARS-CoV-2 infection.
Adaptive Immunity
Antibody/B Cell
Inghirami Laboratory
Our laboratory focuses on dissecting the molecular mechanisms of lymphoid transformation and on identifying the contribution of the host-elements in lymphoid maturation, expansion and viral-tumor immune control. Our research is focused on two directions:
a) Profile serial immune responses using peripheral blood mononuclear cells (PBMC) obtained from SARS-CoV-2-positive individuals (no comorbidities and with cancer) using multicolor flow cytometry, functional and genomic testing (NSG IgH and TCRa/b sequencing). We will take advantage of our existing algorithms to define clonal evolution, and assess the SARS-CoV-2 peptide binding of B- and T-cells. Further studies will determine the binding profile of SARS-CoV2 IgG against a library of recombinant proteins, corresponding to all coding regions of the SARS-CoV2. Predicted anti-SARS-CoV-2 TCR will be cloned and functionally characterized.
b) Generate of an “agnostic” library of human antibodies recognizing multiple SARS-CoV-2 protein epitopes on the viral surface capsid. SARS-CoV-2 specific IgG+ B-cells from convalescent patients (leukapheresis) will be fused to a non-secreting murine myeloma partner to generate human B-cell hybridomas. SARS-CoV-2-specific antibodies will be tested to assess for their binding to Coronovirus proteins (recombinant proteins of 229E, NL63, OC43, HKU1, MERS-CoV, SARS-CoV and SARS-CoV2) and their efficacy in blocking the viral attachment and entry of pseudotyping and natural SARS-CoV-2 to lung epithelial Calu-3 cells.
Melnick Laboratory
The success of vaccines, and effective protection against recurrent infections in general, is dependent on the generation and maintenance of immunological memory, in the form of long-lived plasma cells and Memory B (MB)-cells. MB cells constitute a heterogeneous and quiescent population, poised to quickly respond to antigen upon recall, to provide elevated titers of further specified antibodies. We have defined mechanisms through which somatic mutations in epigenetic regulatory proteins induce lymphomagenesis. Our results show that modulating the primary immune responses through these epigenetic and transcriptional mechanisms in animals results in markedly higher immunoglobulin gene diversity, which could potentially lead to more effective formation of neutralizing antibodies able to clear infections and prevent future re-infections. We have defined specific druggable targets on the regulatory proteins that control this immunoglobulin diversification process. We predict that it will be similarly possible to generate small molecules against these protein domains. We postulate that transient inhibition of these targets can dramatically enhance the humoral immune response to Coronavirus, in the context of primary infections or vaccinations, to favor the development of long-lived MB cells with an extended immunoglobulin gene repertoire. We predict such MB populations would boost the response to ensuing infections with the same or even closely-related virus strains. This approach could enable even cancer patients with impaired humoral immune systems to develop natural immunity to these or other related pathogens.
Mendias Laboratory
We are a translational lab, studying basic biological mechanisms of skeletal muscle and connective tissue growth and remodeling, and applying these to observational studies and clinical trials in patients. A particular focus of our lab is the prevention of skeletal muscle atrophy following injury and disease. Many patients with moderate and severe COVID-19 develop prolong weakness and frailty. The immune system appears to trigger proteolysis in skeletal muscle to mobilize amino acids and energy stores to fuel expansion of immune cell populations and combat acute infection. In patients who experience the most severe frailty and atrophy, immune-mediated muscle proteolysis seems to continue long after the infection has cleared. Previous studies have identified a correlative role of the immune system in inducing muscle atrophy in SARS and MERS patients, although this is unknown in COVID-19 patients. In collaboration with WCM Pathology, we are studying muscle biopsies of COVID-19 patients to identify the nature of weakness and frailty in this disease. We hope these studies will help inform the acute rehabilitation of patients recovering from COVID-19, and identify biological targets for potential interventional trials to restore strength and function.
CD8 T Cell
Blander Laboratory
Our COVID-19 research is centered on testing a novel vaccine candidate, identifying CD8 T cell biomarkers of immune protection, and defining mechanisms of immune evasion and cell death by SARS-CoV-2. We are conducting this work with Weill Cornell Medicine labs of Brad Jones, Laura Santambrogio, Douglas Nixon and Robert Schwartz, Bettina Wagner at Cornell University, and the NYP-WELCOME COVID-19 study by Silvia Formenti, Virginia Pascual and Elizabeth Ross. Our unique contribution to science is discovering the innate immune system can sense microbial viability. We shifted focus in the field from a purely ‘what molecules are there’ to a ‘what is the threat level’ risk assessment of infection. Pathogen-associated molecular patterns (PAMPs) alert the immune system of an infection, but detection of vita-PAMPs signifies a live pathogen and heightens the threat level the immune system is faced with. Bacterial messenger RNA and cyclic dinucleotides are vita-PAMPs that we showed elicit particularly high levels of inflammation and immune protection. We also found that a strategy to block antigen presentation by clinically important viruses, as a means of evading killer CD8 T cells, serves as a proxy of viral viability. It triggers a danger signal in cells to mobilize unconventional traffic of antigen-presenting MHC class I molecules, and activates unique CD8 T cells that protect against the virus. We are positioned to make important discoveries at the leading edge of this frontier in immunology. We are working to incorporate vita-PAMPs and novel adjuvants in vaccines for superior protection against infectious diseases and cancer.
Inghirami Laboratory
Our laboratory focuses on dissecting the molecular mechanisms of lymphoid transformation and on identifying the contribution of the host-elements in lymphoid maturation, expansion and viral-tumor immune control. Our research is focused on two directions:
a) Profile serial immune responses using peripheral blood mononuclear cells (PBMC) obtained from SARS-CoV-2-positive individuals (no comorbidities and with cancer) using multicolor flow cytometry, functional and genomic testing (NSG IgH and TCRa/b sequencing). We will take advantage of our existing algorithms to define clonal evolution, and assess the SARS-CoV-2 peptide binding of B- and T-cells. Further studies will determine the binding profile of SARS-CoV2 IgG against a library of recombinant proteins, corresponding to all coding regions of the SARS-CoV2. Predicted anti-SARS-CoV-2 TCR will be cloned and functionally characterized;
b) Generate of an “agnostic” library of human antibodies recognizing multiple SARS-CoV-2 protein epitopes on the viral surface capsid. SARS-CoV-2 specific IgG+ B-cells from convalescent patients (leukapheresis) will be fused to a non-secreting murine myeloma partner to generate human B-cell hybridomas. SARS-CoV-2-specific antibodies will be tested to assess for their binding to Coronovirus proteins (recombinant proteins of 229E, NL63, OC43, HKU1, MERS-CoV, SARS-CoV and SARS-CoV2;) and their efficacy in blocking the viral attachment and entry of pseudotyping and natural SARS-CoV-2 to lung epithelial Calu-3 cells.
Jones Laboratory
We are a viral immunology lab primarily focused on studying the T cell response to HIV infection, and mechanisms of viral persistence on antiretroviral therapy. We interested in studying how the magnitudes, functionalities, and immunodominance patterns of CD4+ and CD8+ T cell responses to SARS-CoV-2 relate to disease severity and outcome. We are also interested in characterizing the viral dynamics of early SARS-CoV-2 infection in tandem with the cellular immune response. Our lab is also active in performing mouse studies involving replication competent HIV.
Santambrogio Laboratory
Several factors control the outcome of host–viral interactions with host factors being pivotal to both innate and adaptive immunity. Among the host factors that control the end-result of viral infection MHC alleles polymorphism play a fundamental role. The focus of our research will be the characterization of the MHC I and MHC II SARS-CoV-2 immunopeptidome across human ACE2 positive epithelial and endothelial cells as well as professional antigen presenting cells, such as Dendritic Cells which, phagocytose SARS-CoV-2 infected cells and cross-present the antigens to T cells. The ultimate goal would be to comparatively and quantitatively map the differential MHC-restricted immunopeptidome presented by infected cells across different human haplotypes. The top identified antigenic peptides will be tested for recognition by T cells to determine the nature of the T cell response to viral antigens, and to test the hypothesis that certain MHC haplotypes may be protective or conducive of COVID-19 clinical outcome. A well know mechanism of viral escape is the viral interference with the MHC I antigen processing and presentation machinery which generates viral peptides for adaptive immune responses. Indeed, MHC-I viral peptides can stimulate CD8+ cytotoxic T lymphocytes (CTLs), which play a critical role in the defense against viral infections. As part of this project we will also investigate the possibility that SARS-CoV-2 interferes with the proteasome/immunoproteasome or the MHC I assembly trafficking and presentation machinery. Overall, the proposed studies will provide critical information about potential mechanisms of immune escape of SARS-CoV-2.
MHC Peptidome
Blander Laboratory
Our COVID-19 research is centered on testing a novel vaccine candidate, identifying CD8 T cell biomarkers of immune protection, and defining mechanisms of immune evasion and cell death by SARS-CoV-2. We are conducting this work with Weill Cornell Medicine labs of Brad Jones, Laura Santambrogio, Douglas Nixon and Robert Schwartz, Bettina Wagner at Cornell University, and the NYP-WELCOME COVID-19 study by Silvia Formenti, Virginia Pascual and Elizabeth Ross. Our unique contribution to science is discovering the innate immune system can sense microbial viability. We shifted focus in the field from a purely ‘what molecules are there’ to a ‘what is the threat level’ risk assessment of infection. Pathogen-associated molecular patterns (PAMPs) alert the immune system of an infection, but detection of vita-PAMPs signifies a live pathogen and heightens the threat level the immune system is faced with. Bacterial messenger RNA and cyclic dinucleotides are vita-PAMPs that we showed elicit particularly high levels of inflammation and immune protection. We also found that a strategy to block antigen presentation by clinically important viruses, as a means of evading killer CD8 T cells, serves as a proxy of viral viability. It triggers a danger signal in cells to mobilize unconventional traffic of antigen-presenting MHC class I molecules, and activates unique CD8 T cells that protect against the virus. We are positioned to make important discoveries at the leading edge of this frontier in immunology. We are working to incorporate vita-PAMPs and novel adjuvants in vaccines for superior protection against infectious diseases and cancer.
Cantley Laboratory
In collaboration with Blenis, Elemento, Schwartz, Chen Laboratories and with the following laboratories outside of WCM: TenOever (MSSM), Diamond (Washington U), Matthews (Bristol University, UK), Cantley Lab is targeting cellular kinases as treatment for COVID-19. Most cellular processes in human tissues are regulated by Serine/Threonine or Tyrosine protein kinases. In our project, we will test the efficacy of a set of FDA-approved kinase inhibitors on SARS-CoV-2 infection, as well as on the immune response of the host. The set of inhibitors are being chosen based on a new system developed in the Cantley Laboratory for predicting upstream protein kinases for phosphorylation sites. The drugs that block SARS-CoV-2 infectivity as well as modulate the host’s immune response at therapeutically relevant doses will be advanced to clinical trials. In collaboration with Sheinberg Laboratory (MSKCC), the Cantley lab is examining SARS-CoV-2-derived phosphorylated antigen presentation on MHC-I as a vaccine for COVID-19.
Demaria Laboratory
It is expected that many cancer patients will become infected by SARS-CoV-2 and it is essential to understand the interplay of the virus, the immune system and the tumor. A high neutrophil to lymphocyte ratio (NLR) is relatively frequent in patients with some advanced solid malignancies, and is associated with worse outcome. Lymphopenia in cancer patients is also common, often as a result of treatment, and when persistent is usually a negative prognostic indicator. Lymphopenia and high NLR have also been reported in SARS-CoV-2 infected patients. The degree of lymphopenia is associated with disease severity. The exuberant inflammation and immune exhaustion have been hypothesized as causes of the lymphopenia, but the cell subsets most affected and the pathogenesis of lymphopenia remain poorly understood. These observations raise concerns about the risk of severe COVID19 disease in cancer patients, and the modulation of this risk by cancer treatment, including radiotherapy and immunotherapy. Thus, it is critical to better understand the pathogenesis of SARS-CoV-2-driven lymphopenia, and to study whether the immune dysregulation pre-existing in cancer patients alters the development of the immunological changes caused by the infection. As a first step, we plan to investigate possible mechanisms contributing to SARS-CoV-2-driven lymphopenia using in vitro models as well as patients blood and tissue. This hypothesis-generating work will provide the rationale for testing experimentally candidate molecular mechanisms. In parallel, we are interested in understanding whether SARS-CoV-2 infects ACE2-positive cancer cells and can alter the tumor immune contexture.
Santambrogio Laboratory
Several factors control the outcome of host–viral interactions with host factors being pivotal to both innate and adaptive immunity. Among the host factors that control the end-result of viral infection MHC alleles polymorphism play a fundamental role. The focus of our research will be the characterization of the MHC I and MHC II SARS-CoV-2 immunopeptidome across human ACE2 positive epithelial and endothelial cells as well as professional antigen presenting cells, such as Dendritic Cells which, phagocytose SARS-CoV-2 infected cells and cross-present the antigens to T cells. The ultimate goal would be to comparatively and quantitatively map the differential MHC-restricted immunopeptidome presented by infected cells across different human haplotypes. The top identified antigenic peptides will be tested for recognition by T cells to determine the nature of the T cell response to viral antigens, and to test the hypothesis that certain MHC haplotypes may be protective or conducive of COVID-19 clinical outcome. A well know mechanism of viral escape is the viral interference with the MHC I antigen processing and presentation machinery which generates viral peptides for adaptive immune responses. Indeed, MHC-I viral peptides can stimulate CD8+ cytotoxic T lymphocytes (CTLs), which play a critical role in the defense against viral infections. As part of this project we will also investigate the possibility that SARS-CoV-2 interferes with the proteasome/immunoproteasome or the MHC I assembly trafficking and presentation machinery. Overall, the proposed studies will provide critical information about potential mechanisms of immune escape of SARS-CoV-2.
Clonal Hematopoiesis
Lipkin, Hassane and Elemento Laboratories
The presence of clonal hematopoiesis (CH) supports a hyperinflammatory state with elevated cytokines, including IL-1beta and IL-6. Preliminary analysis of macrophages in the lungs of COVID-19 patients with severe disease revealed the presence of more inflammatory macrophages. We hypothesize that CH may underlie the higher incidence of hyperinflammation in susceptible individuals and lead to adverse outcome in COVID-19 patients. We will work to delineate the risk associated with different CH genotypes for COVID-19 related immune-inflammation and elucidate worse clinical outcomes with CH mutations and COVID-19, accounting for lung disease and other predisposing co-morbidities. Finally, to more directly assess the impact on immune-inflammation, we will correlate CH status with plasma cytokine levels (e.g. IL-6).
Underlying Conditions
Obesity
Cohen Laboratory
Faculty including T Krisko and H Nicholls Krisko, and The Metabolic Phenotyping Core Obesity and diabetes are emerging as risk factors for severe COVID-19 complications. This may be related to the influence of obesity on immune function. Our laboratory has extensive experience in animal models of obesity and characterization of associated metabolic abnormalities, including type 2 diabetes and fatty liver disease. We also have extensively characterized the influence of the microbiome on obesity and glucose metabolism. We run the Metabolic Phenotypic Core Facility at WCM, which offers extensive characterization of energy homeostasis, glucose metabolism and body composition. We are well-positioned to examine the influence of COVID-19 on metabolism, as well as the influence of obesity on the course of COVID-19 in suitable mouse models.
Salvatore Laboratory
The clinical spectrum of COVID-19 is heterogeneous and ranges from asymptomatic disease to severe pneumonia and death. COVID-19 patients often have lymphopenia, elevated neutrophils, and increased levels pro-inflammatory cytokines and chemokines. Although age and comorbidities such as diabetes, hypertension and obesity are associated with severe illness, little is known about the determinants of the diverse outcomes. Subjects with hematologic malignancies and/or bone marrow or solid organ transplant are potentially susceptible to severe COVID19, but little is known about the natural history of disease in these patients. To understand the relative contribution of viral evolution and host factors to disease outcome, we built a cohort of patients with varying degree of disease severity that also includes patients with hematologic malignancies and after transplant (in collaboration with H Sing, C Vorkras, JM Hsu, WCM) and we are longitudinally collecting specimens for the comprehensive characterization of viral, epidemiological and immunological drivers of clinical outcome. Our aims are:
1. Profile and characterize cellular and humoral immune responses to SARS-CoV-2, including impact of the virus on immune system (in collaboration with G Inghirami, WCM).
2. Identify the relationships between type of specific immune responses (neutralizing and non-neutralizing antibody, T cells) and subsequent clinical course.
3. Understand the role of deleterious immune responses such as cross-reacting autoantibodies and overly robust cytokines/inflammatory responses in pathogenesis (in collaboration with L Santambrogio WCM and L Ivashkiv, M Crow, HSS).
4. Determine viral dynamics and time of shedding, in different patient populations. (collaboration with E Ghedin, NIH, C Mason, WCM)
Cancer
Demaria Laboratory
Immune dysregulation and lymphopenia in cancer and COVID19 disease
Sandra Demaria, Laura Santambrogio, Mirella Salvatore, Giorgio Inghirami, Sanjay Patel, Silvia Formenti, Shuibing Chen, Robert Schwartz, Massimo Loda, Lewis Cantley
It is expected that many cancer patients will become infected by SARS-CoV-2 and it is essential to understand the interplay of the virus, the immune system and the tumor. A high neutrophil to lymphocyte ratio (NLR) is relatively frequent in patients with some advanced solid malignancies, and is associated with worse outcome. Lymphopenia in cancer patients is also common, often as a result of treatment, and when persistent is usually a negative prognostic indicator. Lymphopenia and high NLR have also been reported in SARS-CoV-2 infected patients. The degree of lymphopenia is associated with disease severity. The exuberant inflammation and immune exhaustion have been hypothesized as causes of the lymphopenia, but the cell subsets most affected and the pathogenesis of lymphopenia remain poorly understood. These observations raise concerns about the risk of severe COVID19 disease in cancer patients, and the modulation of this risk by cancer treatment, including radiotherapy and immunotherapy. Thus, it is critical to better understand the pathogenesis of SARS-CoV-2-driven lymphopenia, and to study whether the immune dysregulation pre-existing in cancer patients alters the development of the immunological changes caused by the infection. As a first step, we plan to investigate possible mechanisms contributing to SARS-CoV-2-driven lymphopenia using in vitro models as well as patients blood and tissue. This hypothesis-generating work will provide the rationale for testing experimentally candidate molecular mechanisms. In parallel, we are interested in understanding whether SARS-CoV-2 infects ACE2-positive cancer cells and can alter the tumor immune contexture.
Formenti Laboratory
Formenti and Marciscano in the Division of Experimental Radiotherapy of the Department of Radiation Oncology are studying the potential to use very low-dose radiation therapy (VLD-RT) as an anti-inflammatory treatment to minimize inflammation and lung injury caused by the SARS-CoV-2 (COVID-19) coronavirus. It has become increasingly clear that the body’s immune response to the virus can become dysregulated leading to life-threatening lung inflammation known as acute respiratory distress syndrome (ARDS). Treatments designed to limit excessive inflammation may help improve outcomes for patients during the COVID-19 pandemic. Historically, VLD-RT was administered to the lungs of patients with severe viral pneumonia that did not respond to standard therapies. Following treatment with VLD-RT, a significant proportion of patients experience rapid improvement in their symptoms. There is now considerable interest in ‘repurposing’ VLD-RT to treat patients with severe pneumonia due to SARS-CoV-2 to prevent the development of ARDS. Human lung cell lines, organoids and in vivo models of severe viral pneumonia/ARDS will help us understand the immunological processes responsible for the immune-suppressive effects of VLD-RT.
We propose to focus on the study of alveolar macrophages (AMs), a potent immune cell population that resides in the respiratory units (alveoli) of the lungs. AMs are a major culprit in ARDS – whether VLD-RT can reprogram AMs towards an anti-inflammatory phenotype that results in less lung injury will be of interest. Furthermore, we will investigate whether VLD-RT modifies expression of ACE2, the receptor that SARS-CoV-2 uses to enter and infect human lung cells (type II pneumocytes).
Melnick Laboratory
The success of vaccines, and effective protection against recurrent infections in general, is dependent on the generation and maintenance of immunological memory, in the form of long-lived plasma cells and Memory B (MB)-cells. MB cells constitute a heterogeneous and quiescent population, poised to quickly respond to antigen upon recall, to provide elevated titers of further specified antibodies. We have defined mechanisms through which somatic mutations in epigenetic regulatory proteins induce lymphomagenesis. Our results show that modulating the primary immune responses through these epigenetic and transcriptional mechanisms in animals results in markedly higher immunoglobulin gene diversity, which could potentially lead to more effective formation of neutralizing antibodies able to clear infections and prevent future re-infections. We have defined specific druggable targets on the regulatory proteins that control this immunoglobulin diversification process. We predict that it will be similarly possible to generate small molecules against these protein domains. We postulate that transient inhibition of these targets can dramatically enhance the humoral immune response to Coronavirus, in the context of primary infections or vaccinations, to favor the development of long-lived MB cells with an extended immunoglobulin gene repertoire. We predict such MB populations would boost the response to ensuing infections with the same or even closely-related virus strains. This approach could enable even cancer patients with impaired humoral immune systems to develop natural immunity to these or other related pathogens.
Inghirami Laboratory
Our laboratory focuses on dissecting the molecular mechanisms of lymphoid transformation and on identifying the contribution of the host-elements in lymphoid maturation, expansion and viral-tumor immune control. Our research is focused on two directions:
a) Profile serial immune responses using peripheral blood mononuclear cells (PBMC) obtained from SARS-CoV-2-positive individuals (no comorbidities and with cancer) using multicolor flow cytometry, functional and genomic testing (NSG IgH and TCRa/b sequencing). We will take advantage of our existing algorithms to define clonal evolution, and assess the SARS-CoV-2 peptide binding of B- and T-cells. Further studies will determine the binding profile of SARS-CoV2 IgG against a library of recombinant proteins, corresponding to all coding regions of the SARS-CoV2. Predicted anti-SARS-CoV-2 TCR will be cloned and functionally characterized;
b) Generate of an “agnostic” library of human antibodies recognizing multiple SARS-CoV-2 protein epitopes on the viral surface capsid. SARS-CoV-2 specific IgG+ B-cells from convalescent patients (leukapheresis) will be fused to a non-secreting murine myeloma partner to generate human B-cell hybridomas. SARS-CoV-2-specific antibodies will be tested to assess for their binding to Coronovirus proteins (recombinant proteins of 229E, NL63, OC43, HKU1, MERS-CoV, SARS-CoV and SARS-CoV2;) and their efficacy in blocking the viral attachment and entry of pseudotyping and natural SARS-CoV-2 to lung epithelial Calu-3 cells.
Chen-Kiang Lab (in collaboration with Olivier Elemento, Giorgio Inghirami and Peter Martin)
We are interested in clonal heterogeneity in lymphoma cells, changes in the immune landscape and tumor - immune interaction in the context of clinical response to our clinical trials targeting BTK and CDK4/6 in lymphoma. We characterize sequential specimens from individual patients by integrated longitudinal functional genomics at single cell resolution, including single cell RNA-seq and IHC and CyTOF. In these studies, we have discovered that the immune components, especially normal B cells, myeloid cells and specific T cell subsets are altered profoundly in lymphoma patients compared with normal individuals, and differentially in responder and non-responders. The outcome of COVID-19 has been reported to be significantly poorer in patients with blood cancers (Leukemia, April 2020). B cells are essential for an antibody response in adaptive immunity in cooperation with cytokines, many of which are produced by monocytes. On this basis, we propose to investigate the role of B cells in COVID-19 outcome in lymphoma patients. We would characterize the immune landscape in PBMC COVID-19 patients with or without lymphoma initially by scRNA-seq in a pilot study, leveraging our substantial scRNA-seq database in lymphoma for computational analysis in the context of outcome and antibody production. We will then pursue the most promising leads in B cells and monocytes and develop cost-effective IHC or CyTOF analysis to address whether and how impairment in the immune system by cancer exacerbates the disease severity in COVID-19.
Co-Infection
Iliev Laboratory and Worgall Laboratory
We will investigate the role of the mycobiome/lung fungal co-infection in development and rapid exacerbation (or lack of such) of COVID-19 disease. Patient sputum, lung aspirates and fecal samples will be used to uncover fungal players, fungal immune signatures and lipid metabolites associated with disease outcome. The study will benefit from several advanced mycobiome and immuno-mycology pipelines in the Iliev laboratory, lipid metabolism expertise and tools available in the Worgall Laboratory. Mechanisms of disease severity will be further investigated in mouse models.
Inghirami Laboratory
Our laboratory focuses on dissecting the molecular mechanisms of lymphoid transformation and on identifying the contribution of the host-elements in lymphoid maturation, expansion and viral-tumor immune control. Our research is focused on two directions:
a) Profile serial immune responses using peripheral blood mononuclear cells (PBMC) obtained from SARS-CoV-2-positive individuals (no comorbidities and with cancer) using multicolor flow cytometry, functional and genomic testing (NSG IgH and TCRa/b sequencing). We will take advantage of our existing algorithms to define clonal evolution, and assess the SARS-CoV-2 peptide binding of B- and T-cells. Further studies will determine the binding profile of SARS-CoV2 IgG against a library of recombinant proteins, corresponding to all coding regions of the SARS-CoV2. Predicted anti-SARS-CoV-2 TCR will be cloned and functionally characterized;
b) Generate of an “agnostic” library of human antibodies recognizing multiple SARS-CoV-2 protein epitopes on the viral surface capsid. SARS-CoV-2 specific IgG+ B-cells from convalescent patients (leukapheresis) will be fused to a non-secreting murine myeloma partner to generate human B-cell hybridomas. SARS-CoV-2-specific antibodies will be tested to assess for their binding to Coronovirus proteins (recombinant proteins of 229E, NL63, OC43, HKU1, MERS-CoV, SARS-CoV and SARS-CoV2;) and their efficacy in blocking the viral attachment and entry of pseudotyping and natural SARS-CoV-2 to lung epithelial Calu-3 cells.
Ndhlovu Laboratory
My research program uses single cell and immuno-epigenetic approaches to resolve molecular mechanisms regulating viral entry of SARS-CoV-2 infection across various tissues and cell types and seeks to identify therapeutic host targets that influence disease pathogenesis and reduce morbidity and mortality and relieve the burden of this infection.
Nixon Laboratory
My lab is interested in collaborating on basic host pathogen interactions in the context of SARS-CoV-2 and HIV co-infection, and on the genetics of COVID-19 susceptibility and disease progression. We also have used connectivity mapping for drug repurposing studies in COVID-19. We are also interested in how innate iNKT and MAIT immune cells might contribute to pathogenesis or protection.
Josefowicz Laboratory
Epigenetic Priming of Inflammatory Genes in COVID-19: Insights into Pathogenesis, Prognosis, and Consequences. A major priority is to understand the inflammatory pathology of COVID-19. The urgent applications of that knowledge would include identification of novel therapeutic targets, risk stratification especially among those that are otherwise young and healthy, and guiding of existing experimental therapies such as cytokine blockade. Our approach is to profile epigenetic priming of inflammatory genes in immune cells using low cell number epigenomics, with the hypothesis that epigenetic “poising” at inflammatory genes contributes to COVID-19 course. We have already established this workflow in studies of inflammatory arthritis (collaboration with Virginia Pascual) to study the relationship between inflammatory gene poising and disease states and responsiveness to immune therapies, and also to understand the range of epigenetic poising of inflammation among healthy donors and across age and sex. These studies focus on underlying mechanisms of inflammatory pathology and their long-term sequelae with relevance extending beyond COVID-19 to a broad array of disease states, including other respiratory infections, ARDS, and inflammatory disease, and what we learn could have long-term benefit across a range of conditions.
IBD
Artis Laboratory
We study the regulation of innate and adaptive immunity at the body’s barrier surfaces, including the airway and intestine, in the context of infection, inflammation and tissue repair. We also employ experimental techniques to examine how the microbiota that colonize these barrier surfaces influence immunity and inflammation. In the context of anti-viral immunity, we previously identified a critical role for signals derived from the microbiota in promoting innate and adaptive immunity to influenza, LCMV and norovirus. Given the high levels of SARS-CoV-2 in the human intestine along with expression of receptors for cell entry, we would propose to study associations between microbial diversity within the microbiota of patients and susceptibility to SARS-CoV-2 infection and disease severity. We also established the Roberts Institute Live Cell Bank that routinely collects clinical data, matched blood, intestinal biopsies and microbiota samples. This resource could be applied to multiple SARS- CoV-2 studies.
Cohen Laboratory
Faculty including T Krisko and H Nicholls Krisko, and The Metabolic Phenotyping Core Obesity and diabetes are emerging as risk factors for severe COVID-19 complications. This may be related to the influence of obesity on immune function. Our laboratory has extensive experience in animal models of obesity and characterization of associated metabolic abnormalities, including type 2 diabetes and fatty liver disease. We also have extensively characterized the influence of the microbiome on obesity and glucose metabolism. We run the Metabolic Phenotypic Core Facility at WCM, which offers extensive characterization of energy homeostasis, glucose metabolism and body composition. We are well- positioned to examine the influence of COVID-19 on metabolism, as well as the influence of obesity on the course of COVID-19 in suitable mouse models.
Guo Laboratory
About 20% of COVID-19 patients have diarrhea as the first symptom, suggesting a compositional and functional change of their gut microbiota. We are a gut microbiome lab that uses genetic approaches to modulate gut microbiota and investigate how their genes, pathways, and metabolites affect host biology. We are interested to know how the viral infection modifies the gut microbiota at the molecular level that leads to diarrhea, and we seek to engineer the human gut microbiota for better protection against Covid-19 or to ameliorate COVID-19 related diarrhea. My group is also open to other collaboration opportunities as long as our expertise can contribute.
Longman Laboratory
Our laboratory has experience in immunophenotyping and microbiome analysis of patients with inflammatory bowel disease (IBD). Diarrhea and GI symptoms are common presenting symptoms of COVID-19, but the impact on intestinal homeostasis, the effect on underlying IBD, and the interaction with immunosuppressive medications is not known. We have developed longitudinal clinic-based treatment cohorts that can be used to examine these questions in patients with IBD.
Sonnenberg Laboratory
The Sonnenberg Laboratory has substantial expertise in defining the cellular and molecular mechanisms by which host-microbe interactions augment immunity, inflammation, tissue homeostasis and cancer within the mammalian gastrointestinal tract. Particularly, we focus on how the mammalian immune system interacts with trillions of normally beneficial microbes, termed the microbiota, to support intestinal health. The recent SARS-CoV-2 pandemic has demonstrated that this infection is commonly associated with multiple gastrointestinal symptoms, such as loss of appetite, nausea, vomiting and diarrhea. Furthermore, the virus is regularly detected in the feces of infected patients. Therefore, we are actively interrogating: (i) How SARS-CoV-2 infection causes gastrointestinal disorders; (ii) Whether there are long-term immunologic or microbiologic changes in the human intestine following SARS-CoV-2 infection; and (iii) Can we develop novel therapeutic approaches to protect the gastrointestinal tract in the context SARS-CoV-2 infection and enhance protective immunity. These research efforts are in close collaboration with multiple investigators at the Roberts Institute for Research in IBD, the Department of Medicine, and the Division of Gastroenterology.
Autoimmunity
Pernis Laboratory
Studies in aging mice have identified a B cell subset, termed Age-associated/Autoimmune B cells (ABCs), which, in addition to classical B cell markers, also express myeloid markers. Expansion of ABCs is normally triggered by viral infections such as flu. ABCs aberrantly accumulate in autoimmune disorders like SLE, where they rapidly differentiate into plasma cells and are major producers of autoantibodies including anti-phospholipid antibodies. Our laboratory has utilized a murine model to study ABCs and has found that the generation, differentiation, and function of ABCs are differentially controlled in females and males. We have furthermore found that their expansion and function can be promoted by ingestion of a Western diet. We are thus well-positioned to help investigate how sex-differences and dyslipidemia can contribute to the pathogenesis of COVID-19.
Lu Laboratory
Our lab studies how immune cells modulate and are modulated by tissue-resident cells, with a focus on understanding rheumatic diseases such as lupus, where patients develop skin lesions in the sun and this can trigger an increase in their autoimmune responses. We are interested in how inflammation in the skin and other tissues can modulate immune responses that begin in lymphoid organs such as lymph nodes and tonsils. We are interested in how inflammation in COVID-19 infections impacts immune responses initiated in lymphoid organs and how understanding COVID-19 can inform and be informed by understanding of rheumatic diseases.
Age, Pregnancy, and Gender
Pascual Laboratory
Virginia Pascual’s group is working on an NIAID Supplement to 5 U01 AI1131386-03 (High Precision Systems Analysis of Infant Immune Responses; O. Ramilo P.I. Nationwide, Columbus, OH; V Pascual, Co-I): This supplement intends to recruit 200 pregnant mother-infant pairs in the US and Central America (Panama), where a network of pediatricians involved in maternal-fetal immune monitoring is already in place. The goal of this proposal is to comprehensively characterize the clinical, immunologic, viral variables and outcomes of COVID-19 infection in mother-infant pairs and to assess the development of the immune system during the 1st year of life.
We are also working on a collaboration with Steve Josefowicz’s group to examine the role of “Trained Immunity” in predisposition to severe COVID-19 outcome. The proposal is based on preliminary data obtained as a collaboration between our labs addressing how epigenetic reprogramming of innate immune precursors might predispose children with autoinflammatory diseases to exaggerated responses to subsequent inflammatory triggers. The hypothesis is that COVID-19 patients suffering from “cytokine storms” are epigenetically predisposed to innate immunity-related morbidity.
Finally, we are involved in the development phase of “WelCoME-C: Weil Cornell Medicine Employees Cohort”. This protocol, led by Silvia Formenti, intends to develop a longitudinal cohort to capture Weill-Cornell Medicine employees through SARS-CoV-2 exposure. The goals are to integrate clinical, laboratory, virus-related factors, demographics and comorbidities. Importantly, it will acquire and store samples for viral studies, genetic associations as well as immune monitoring to identify predictors of outcomes.
Pernis Laboratory
Studies in aging mice have identified a B cell subset, termed Age-associated/Autoimmune B cells (ABCs), which, in addition to classical B cell markers, also express myeloid markers. Expansion of ABCs is normally triggered by viral infections such as flu. ABCs aberrantly accumulate in autoimmune disorders like SLE, where they rapidly differentiate into plasma cells and are major producers of autoantibodies including anti-phospholipid antibodies. Our laboratory has utilized a murine model to study ABCs and has found that the generation, differentiation, and function of ABCs are differentially controlled in females and males. We have furthermore found that their expansion and function can be promoted by ingestion of a Western diet. We are thus well-positioned to help investigate how sex-differences and dyslipidemia can contribute to the pathogenesis of COVID-19.
Zeng Laboratory
We are a gut microbiome immunology lab with a focus on neonatal immunity against infections and the immune response at the maternal-fetal/neonatal interface. We also have ongoing studies of the neonatal gut microbiome in both humans and mice. Our interests center on defining whether there are immune or gut microbiome components that modulate vertical transmission of SARS-CoV-2 from the mother to the fetus or newborn. Utilizing novel COVID-19 mouse models with either neutrophil deficiency or IgG deficiency, we would like to define the contribution of neutrophils and the role of non-neutralizing IgG in the “cytokine storm”. In understanding why children have mild symptoms of SARS-CoV-2 infection, we plan on exploring potential unique gut microbiome-derived factors that confer protection in children. We are interested in the role of the gut microbiome in SARS-CoV-2 infection.
Metabolism
Cohen Laboratory
Faculty including T Krisko and H Nicholls Krisko, and The Metabolic Phenotyping Core Obesity and diabetes are emerging as risk factors for severe COVID-19 complications. This may be related to the influence of obesity on immune function. Our laboratory has extensive experience in animal models of obesity and characterization of associated metabolic abnormalities, including type 2 diabetes and fatty liver disease. We also have extensively characterized the influence of the microbiome on obesity and glucose metabolism. We run the Metabolic Phenotypic Core Facility at WCM, which offers extensive characterization of energy homeostasis, glucose metabolism and body composition. We are well-positioned to examine the influence of COVID-19 on metabolism, as well as the influence of obesity on the course of COVID-19 in suitable mouse models.
Prospective Study
NYP-WELCOME
(NYP-Weill Cornell Medicine Employees)
Silvia C Formenti, Viginia Pascual and Elizabeth M. Ross
COVID-19, is the highly infectious disease caused by a new virus, SARS-CoV-2, and it manifests in different forms of severity. The majority of people who contract the infection either have no symptoms or mild ones, similar to a febrile upper respiratory infection and/or a bowel infection. Most cases recover within a few days. However, in 5% of COVID-19 patients there is need for hospital admission with risk of mortality. At this point however, physicians and scientists are unable to predict who is at risk of dying of COVID-19. We hypothesize that NYP-Weill Cornell Medicine asymptomatic healthcare workers (HCW) can be studied over time to learn about the many determinants of COVID-19 outcome. Consented volunteers will provide basic clinical information and undergo multiple sequential testing to assess if they are infected by the virus and to monitor the development of an immune response to the virus. Volunteers will donate specimens (blood, saliva, stool, urine) for diagnostic testing and for biomedical research on COVID-19.
The aims are:
1. To characterize the natural history of COVID-19 over time, from community exposure to disease outcome in a prospective HCW cohort of 1000 individuals asymptomatic at baseline (WELCOME cohort).
2. To generate an annotated biospecimens repository (a bank of the collected tissues, annotated with basic clinical information), made unidentifiable and available to the scientific community for studying COVID-19.
3. To perform genetic and immunological studies to explore whether there is a genetic predisposition to the different forms of COVID-19 disease.
4. To explore the consequences of COVID-19 on the quality of life of HCW.