Diversity at Weill Cornell Medicine
- Cornell University Center for Health Equity: This initiative between Weill Cornell Medicine and Cornell University seeks to enhance healthcare and health equity through research, education, and advocacy, all in partnership with the community.
- Weill Cornell Medicine Diversity Mission: WCM values diversity. Conducting research that benefits all members of the community.
- Weill Cornell Medicine Office of Diversity and Inclusion: The mission of the Office of Diversity and Inclusion at Weill Cornell Medical College is to foster an atmosphere in which individual characteristics are respected and where both differences and similarities are valued.
- Affinity Groups and Diverse Communities at WCM: Our diverse medical communities help to ensure the best possible care, research and education at Weill Cornell Medicine. Community engagement efforts and 'Tri-I' group programs are two of the most important ways that we maintain diversity.
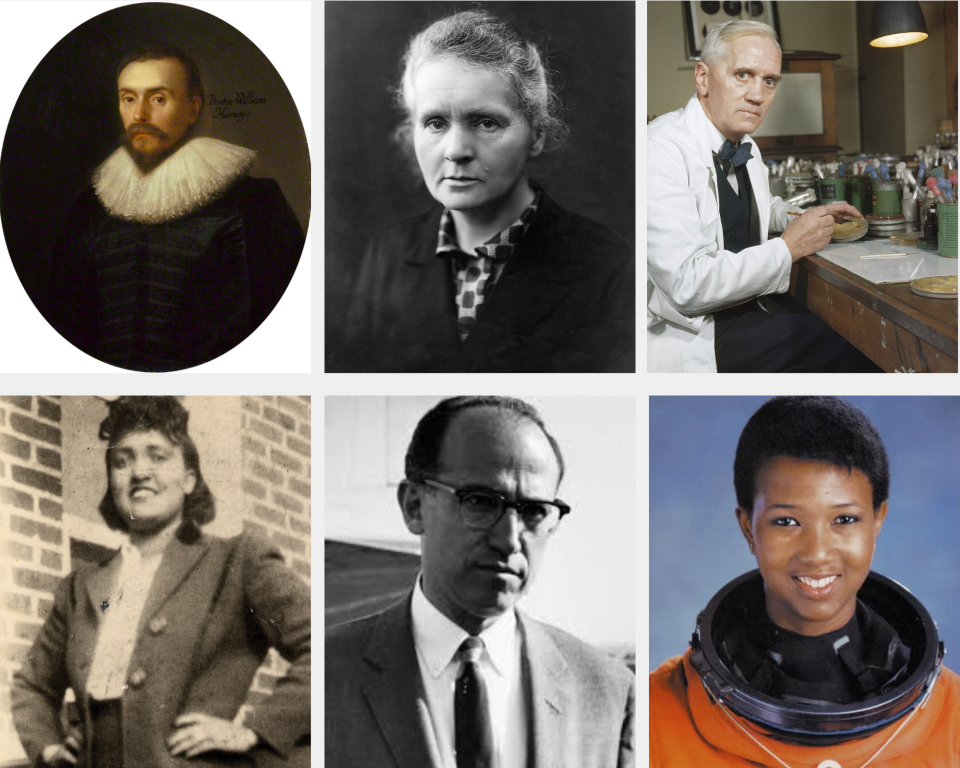
Celebrating the Scientific Workforce
Science is a diverse plethora of unique organisms, genes, and characteristics, much like the people who contribute to breakthroughs and revolutionary care. For science to thrive, so must the people.

Informational Resources about Health Disparities, Equity and Minority Health in the United States
The following informational resources from nationally-recognized organizations and entities provide useful, evidence-based statistics on the health disparities between racial groups across the United States.

Dr. Nikolaos Koundouros, Postdoctoral Associate in the Laboratory of Dr. John Blenis
Tri-Institutional Breakout Award for Junior Investigators
Weill Cornell Medicine, Memorial Sloan Kettering Cancer Center and The Rockefeller University present the awards to up to six exceptional investigators each year—at least one from each institution—who are recognized for their notable research achievements, impactful findings and high potential for success as independent investigators. Winners receive a $25,000 unrestricted prize.
Dr. Nikolaos Koundouros, a postdoctoral associate in the Department of Pharmacology is the 2025 Tri-Institutional Breakout Award for Junior Investigators from Weill Cornell Medicine. Dr. Koundouros earned his doctorate at the Institute of Cancer Research in London, during which time he helped pioneer the use of a surgical tool called the iKnife that can detect cancer by analyzing tissue chemistry in real time. He also uses advanced tools and techniques to measure how cells break down sugars and fats. His work has fueled the creation of a potential cancer treatment that targets how cells detect nutrients. Continue reading at the WCM Newsroom
Ritu Banga Healthcare Disparities Research Awards
Generously endowed by Ritu and Board Fellow Ajay Banga, the awards will support excellence in research to improve the health of women and underrepresented minorities and/or to reduce health disparities in healthcare systems and clinical settings, either locally or globally.
The awards are designed to further Weill Cornell Medicine’s goal of becoming a national leader in advancing diversity, inclusion, and gender equity within academic medicine. We seek proposals for basic, translational, clinical, informatics, or outcomes research that addresses health disparity areas including, but not limited to race and ethnicity, gender and gender identity, socioeconomic status, access to healthcare, differing standards of healthcare, insurance status, age, geography, sexual orientation, and cultural beliefs. Projects that enhance the diversity pipeline either through research or the inclusion of diverse personnel are also encouraged.
