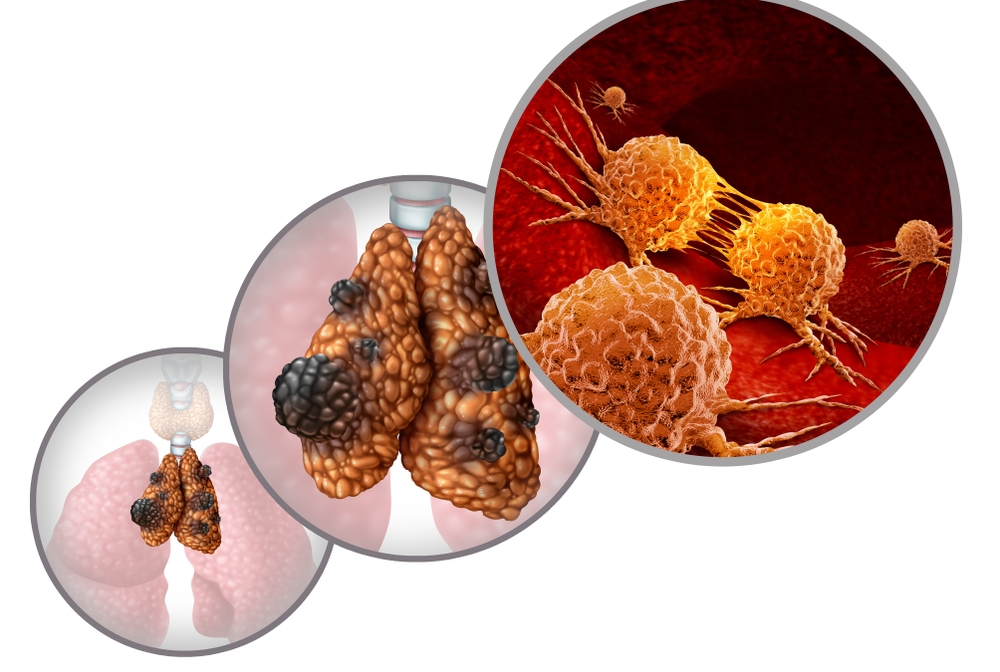
A new preclinical model for thymic cancer developed by Weill Cornell Medicine investigators has revealed insights into how a common mutation found in thymic epithelial tumors sparks their formation. The model may help speed the development of targeted therapies for cancer of the thymus, a gland that makes immune cells that help protect the body from infections.
In a study published Aug. 29 in the Journal of Thoracic Oncology, senior author Dr. Giuseppe Giaccone, professor of medicine and associate director of clinical research at the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine, and his colleagues describe a genetically engineered mouse model in which the animals’ thymic epithelial cells harbor a genetic variant called GTF2I L424H, the most common mutation in thymic cancers.
“Having a mouse model of thymic epithelial tumors will help us learn more about how these tumors form and allow us to test new therapies,” said Dr. Giaccone, who is also an oncologist at NewYork-Presbyterian/Weill Cornell Medical Center.
The study’s lead author Dr. Yongfeng He, instructor of cancer biology in medicine at Weill Cornell Medicine, explained that thymic cancers are a rare, complex and understudied type of cancer. Certain autoimmune conditions are associated with thymic epithelial tumors, but the reason why is unclear. There are currently no good preclinical models that recreate the disease features in humans, and only a handful of cell lines are available for study, he said.
This lack of experimental models has hampered research on new therapies for the condition. Surgery is usually the first-choice treatment, but if that fails, patients with thymic cancer may undergo chemotherapy, immunotherapy or other targeted therapies developed for different cancers. However, these second-line therapies aren’t curative, Dr. Giaccone said.
“We wanted to understand why these tumors happen and how we can develop curative therapies,” Dr. He said.
The team genetically engineered mice to have the GTF2I L424H mutation in thymic epithelial cells and found abnormal development of the cells in young animals. As the animals age, they develop tumors in their thymus. They found that expression of many genes involved in the production of new thymic cells are altered in the mice, including genes previously implicated in other cancers. When the team compared the mouse tumors with human thymic cancer samples, they found that the mouse tumors share many molecular characteristics with type B1 and B2 human thymic tumors.
“We think the GTF2I L424H mutation starts the process of tumor formation,” Dr. Giaccone said. “Adding more mutations may make the tumors more aggressive.”
The next step for the team will be studying precisely how this mutation causes cancerous changes in the thymus and what other genetic pathways are involved, Dr. He said. Because the gene affected by the GTF2I L424H mutations controls the expression of many other genes, Dr. He said it is probably not a good target for anti-cancer therapies. But some of the other genes it turns on or off might be potential targets.
“We can use our mouse model to test drugs that target these other genes to find better therapies specific to thymic epithelial tumors,” Dr. He said.
