Stimulating a key metabolic pathway in T cells can make them work more effectively against tumors when combined with immune checkpoint inhibitor therapy, according to a preclinical study led by researchers at Weill Cornell Medicine. The findings suggest a potential strategy for enhancing the potency of anticancer immunotherapies.
In the study, which appears Sept. 26 in Nature Immunology, the researchers discovered that activating a metabolic pathway called the pentose phosphate pathway makes antitumor CD8 T cells more likely to stay in an immature, stem-like, “precursor” state. They showed that combining this metabolic reprogramming of T cells with a standard anticancer immune checkpoint inhibitor treatment leads to big improvements in tumor control in animal models and in tumor “organoids” grown from human tumor samples.

Dr. Vivek Mittal
“Our hope is that we can use this new metabolic reprogramming strategy to significantly boost patients’ response rates to immune checkpoint inhibitor therapies,” said study senior author Dr. Vivek Mittal, the Ford-Isom Research Professor of Cardiothoracic Surgery at Weill Cornell Medicine.
The study’s lead author was Dr. Geoffrey Markowitz, a postdoctoral research associate in the Mittal laboratory.
T cells and other immune cells, when active, eventually start to express immune-suppressing checkpoint proteins such as PD-1, which are thought to have evolved to keep immune responses from running out of control. Within the past decade, immunotherapies that boost anticancer immune responses by blocking the activity of these checkpoint proteins have had some astounding successes in patients with advanced cancers. However, despite their promise, checkpoint inhibitor therapies tend to work well for only a minority of patients. That has spurred cancer biologists to look for ways of boosting their performance.
In the new study, the researchers began by examining gene activity in cancer-fighting T cells within tumors, including tumors subjected to PD-1-blocking drugs. They found a puzzling connection between higher T-cell metabolic gene activity and lower T-cell effectiveness at fighting tumors.
The researchers then systematically blocked the activity of individual metabolic genes and discovered that blocking the gene for a metabolic enzyme called PKM2 had a remarkable and unique effect: It boosted the population of a less mature, precursor type of T cell, which can serve as a long-term source of more mature tumor-fighters called cytotoxic CD8+ T cells. This enzyme had also been identified in prior studies as more likely to produce effective antitumor responses in the context of anti-PD1 treatment.
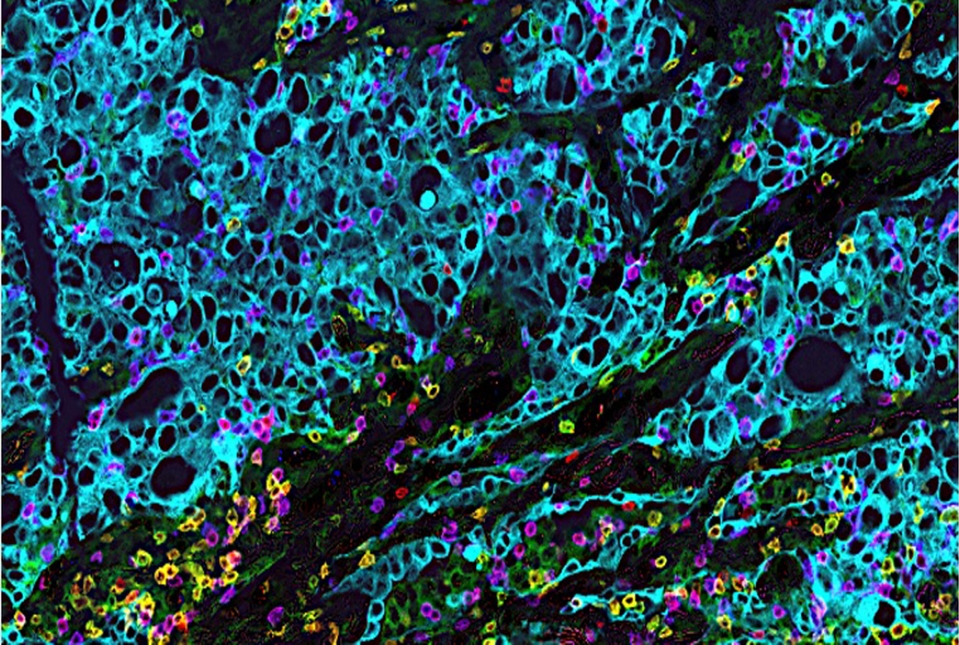
The researchers showed that the enhanced presence of these precursor T cells did indeed bring better results in animal models of anti-PD-1-treated lung cancer and melanoma, and in a human-derived organoid model of lung cancer.
“Having more of these precursors enables a more sustained supply of active cytotoxic CD8+ T cells for attacking tumors,” said Dr. Mittal, who is also a member of the Sandra and Edward Meyer Cancer Center and the Englander Institute for Precision Medicine at Weill Cornell Medicine.
The researchers found that blocking PKM2 exerts this effect on T cells mainly by boosting a metabolic pathway called the pentose phosphate pathway, whose multiple functions include the generation of building blocks for DNA and other biomolecules.
“We found that we could reproduce this reprogramming of T cells just by activating the pentose phosphate pathway,” Dr. Markowitz said.
The researchers currently are conducting further studies to determine more precisely how this reprogramming occurs. But their findings already point to the possibility of future treatments that would alter T cells in this way to make them more effective tumor fighters in the context of checkpoint inhibitor therapy. Drs. Markowitz and Mittal and their colleagues are currently discussing with the Sanders Tri-Institutional Therapeutics Discovery Institute a project to develop agents that can induce T-cell-reprogramming for use in future clinical trials.
Dr. Markowitz noted that the strategy might work even better for cell-transfer anticancer therapies such as CAR-T cell therapies, which involve the modification of the patient’s T cells in a laboratory setting followed by the cells’ re-infusion into the patient.
“With the cell transfer approach, we could manipulate the T cells directly in the lab dish, thereby minimizing the risk of off-target effects on other cell populations,” he said.
